Antipests
< DRAFT++ >
Biting, stinging, parasiting, blood-stucking, skin-burrowing, egg-laying, virus-carrying, zoonotic, contaminating, toxifying...
Revisions:
xxxxxxxx
20191109 reorg at cht7a
20200511 touch
20200820 overview
20201017 ping + new sea biters + parasites reorg
20230225 (recent work around Cuba)
Ties to:
🔗medical
———————— specific
🔗antiticks
🔗toxoplasmosis
🔗pandemic
###
Table of Contents
¶FLEAS
esp: "Pulgas"
slo: "Bolhe"
___________
* Cat flea vs Dog flea vs Human flea
* Dog flea:
It closely resembles the cat flea, Ctenocephalides felis, which can live on a wider range of animals and is generally more prevalent worldwide.[1]
* Cat flea:
"""The cat flea affects both the cat and the dog worldwide.[5] The cat flea can also maintain its life cycle on other carnivores and on omnivores, but these are only chosen when more acceptable hosts become unavailable.[4] Adult cat fleas do not willingly leave their hosts, and inter-animal transfer of adult fleas is rare except in animals that share sleeping quarters. A flea which becomes separated from its host will often die within hours from starvation.[6]"""
* Only bite around ankles (?)
* "The bite site has a single puncture point in the center. Bites often appear in clusters or small rows and can remain inflamed for up to several weeks. "
* """This species bites many species of mammals and birds, including domesticated ones. It has been found on dogs and wild canids, monkeys in captivity, opossums, domestic cats, wild felids in captivity, chickens, black rats and Norwegian rats, wild rodents, pigs, free-tailed bats, and other species. It can also be an intermediate host for the flea tapeworm cestode Dipylidium caninum.
Fleas can spread rapidly and move between areas to include eyebrows, eyelashes, and pubic regions. """
___________
https://en.wikipedia.org/wiki/Pulicosis
esp: "Pulgas"
slo: "Bolhe"
___________
* Cat flea vs Dog flea vs Human flea
* Dog flea:
It closely resembles the cat flea, Ctenocephalides felis, which can live on a wider range of animals and is generally more prevalent worldwide.[1]
* Cat flea:
"""The cat flea affects both the cat and the dog worldwide.[5] The cat flea can also maintain its life cycle on other carnivores and on omnivores, but these are only chosen when more acceptable hosts become unavailable.[4] Adult cat fleas do not willingly leave their hosts, and inter-animal transfer of adult fleas is rare except in animals that share sleeping quarters. A flea which becomes separated from its host will often die within hours from starvation.[6]"""
* Only bite around ankles (?)
* "The bite site has a single puncture point in the center. Bites often appear in clusters or small rows and can remain inflamed for up to several weeks. "
* """This species bites many species of mammals and birds, including domesticated ones. It has been found on dogs and wild canids, monkeys in captivity, opossums, domestic cats, wild felids in captivity, chickens, black rats and Norwegian rats, wild rodents, pigs, free-tailed bats, and other species. It can also be an intermediate host for the flea tapeworm cestode Dipylidium caninum.
Fleas can spread rapidly and move between areas to include eyebrows, eyelashes, and pubic regions. """
___________
https://en.wikipedia.org/wiki/Pulicosis
¶BED BUGS
aka bedbugs
esp: "Chinche (de las camas)"
lat: Cimicidae
slo: "Stenice"
___________
best resources:
* https://www.reddit.com/r/Bedbugs (sticky posts!!)
* http://www.bedbug-answers.com/signs-of-bed-bugs.html?fbclid=IwAR2FAfqkJzmsS60oVL3f8HpCmnmO5lhwufAMImMM-idfZrokCkEkI-Zu5YQ
* ID + common misidentifications:
https://www.reddit.com/r/Bedbugs/comments/2y4ll3/bedbug_id_and_common_misidentifications/
book lice nymphs :p
* [...]
_______________________
* Can you starve them out?
"Newly hatched nymphs must consume a blood meal within two to three days or will die of starvation, whereas an adult can live for as long as six months between feedings.[7]"
"In some studies, bed bugs have been documented to live for up to 18 months without feeding. In other studies, they’ve lasted only 4-6 months."
* They only feed at night !
* Natural remedies:
* Tea tree oil
* Lavender
* [...]
* Eliminate:
* Freezing the bedding, pillow and bed covers in extreme cold for 48 to 72 hours can help eliminate these pests.
* Professional bed bug exterminators use:
* carbon dioxide under pressure to immediately eliminate bed bugs and their eggs
* Steam heating is another effective method
________________
* they leave bloodstains on the sheets !
* "While visiting, sit on a non-upholstered chair if possible, such as a wooden dining chair. Bed bugs often hide inside couches."
* "Bedbugs don’t live on people permanently like lice"
_________
* use mattress encasements !
https://www.bedbugsinsider.com/do-bed-bug-mattress-covers-work/
https://www.thesleepjudge.com/roundup/best-mattress-encasement-reviews/
>pau #hypertextile
what are they made out of ?
________
"""Bed bugs can survive for a long time without oxygen. When inside a completely airtight container, they can live for up to 5 days. And of course, if there’s even the smallest hole in the container, this will provide them with enough air to live on."""
"""Groups of tiny dark spots that smear when they are wiped with a wet rag. This is bed bug fecal matter and is generally dark brown or black in color."""
___________
* good resource:
https://www.bedbugsinsider.com/my-friend-has-bed-bugs/
* good photos for identification on mattresses:
https://extension.entm.purdue.edu/publichealth/insects/bedbug.html
* DETECTION:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3617843/
Bed Bug Detection: Current Technologies and Future Directions
https://www.sciencemag.org/news/2019/05/bedbugs-date-back-time-dinosaurs-new-family-tree-suggests
good article on where they come from - GUANO MINING !
"""
Since then, one or two other bedbug species have switched to human hosts, Reinhardt says. For example, his research on Hopi legends has convinced him that a bedbug known to infect eagles also started to feed on humans. And the human-loving bedbug Leptocimex boueti, which also enjoys bat blood and likely had that mammal as its first host, may have switched to people as global guano mining increased
"""
https://www.livescience.com/42297-bed-bugs-facts-information.html
good overal view
_____________
"""
Cimex lectularius is a species of Cimicidae (bed bugs). Its primary hosts are humans, and it is one of the world's major "nuisance pests".
"""
esp: "Chinche (de las camas)"
lat: Cimicidae
slo: "Stenice"
___________
best resources:
* https://www.reddit.com/r/Bedbugs (sticky posts!!)
* http://www.bedbug-answers.com/signs-of-bed-bugs.html?fbclid=IwAR2FAfqkJzmsS60oVL3f8HpCmnmO5lhwufAMImMM-idfZrokCkEkI-Zu5YQ
* ID + common misidentifications:
https://www.reddit.com/r/Bedbugs/comments/2y4ll3/bedbug_id_and_common_misidentifications/
book lice nymphs :p
* [...]
_______________________
* Can you starve them out?
"Newly hatched nymphs must consume a blood meal within two to three days or will die of starvation, whereas an adult can live for as long as six months between feedings.[7]"
"In some studies, bed bugs have been documented to live for up to 18 months without feeding. In other studies, they’ve lasted only 4-6 months."
* They only feed at night !
* Natural remedies:
* Tea tree oil
* Lavender
* [...]
* Eliminate:
* Freezing the bedding, pillow and bed covers in extreme cold for 48 to 72 hours can help eliminate these pests.
* Professional bed bug exterminators use:
* carbon dioxide under pressure to immediately eliminate bed bugs and their eggs
* Steam heating is another effective method
________________
* they leave bloodstains on the sheets !
* "While visiting, sit on a non-upholstered chair if possible, such as a wooden dining chair. Bed bugs often hide inside couches."
* "Bedbugs don’t live on people permanently like lice"
_________
* use mattress encasements !
https://www.bedbugsinsider.com/do-bed-bug-mattress-covers-work/
https://www.thesleepjudge.com/roundup/best-mattress-encasement-reviews/
>pau #hypertextile
what are they made out of ?
________
"""Bed bugs can survive for a long time without oxygen. When inside a completely airtight container, they can live for up to 5 days. And of course, if there’s even the smallest hole in the container, this will provide them with enough air to live on."""
"""Groups of tiny dark spots that smear when they are wiped with a wet rag. This is bed bug fecal matter and is generally dark brown or black in color."""
___________
* good resource:
https://www.bedbugsinsider.com/my-friend-has-bed-bugs/
* good photos for identification on mattresses:
https://extension.entm.purdue.edu/publichealth/insects/bedbug.html
* DETECTION:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3617843/
Bed Bug Detection: Current Technologies and Future Directions
https://www.sciencemag.org/news/2019/05/bedbugs-date-back-time-dinosaurs-new-family-tree-suggests
good article on where they come from - GUANO MINING !
"""
Since then, one or two other bedbug species have switched to human hosts, Reinhardt says. For example, his research on Hopi legends has convinced him that a bedbug known to infect eagles also started to feed on humans. And the human-loving bedbug Leptocimex boueti, which also enjoys bat blood and likely had that mammal as its first host, may have switched to people as global guano mining increased
"""
https://www.livescience.com/42297-bed-bugs-facts-information.html
good overal view
_____________
"""
Cimex lectularius is a species of Cimicidae (bed bugs). Its primary hosts are humans, and it is one of the world's major "nuisance pests".
"""
¶LICE + NITS
esp: "Piojos & Liendres"
slo: "Uši & Gnide"
_______________
* live on people permanently
https://en.wikipedia.org/wiki/Pediculus_humanus
body lice, head lice
___________
treatment
* get a special comb (metallic)
* repel with tea tree oil
#tomerge
with d experience post 35c3
esp: "Piojos & Liendres"
slo: "Uši & Gnide"
_______________
* live on people permanently
https://en.wikipedia.org/wiki/Pediculus_humanus
body lice, head lice
___________
treatment
* get a special comb (metallic)
* repel with tea tree oil
#tomerge
with d experience post 35c3
¶TICKS
esp: "Garrapatas"
slo: "Klopi"
lat: "Ixodoidea"
___________________
→ 🔗antiticks
#tomerge [!!*]
* https://www.sos-klop.si/klopi-v-sloveniji [SLO]
* ###
esp: "Garrapatas"
slo: "Klopi"
lat: "Ixodoidea"
___________________
→ 🔗antiticks
* https://www.sos-klop.si/klopi-v-sloveniji [SLO]
* ###
¶MOSQUITOS
Repelling:
* Similar to ticks:
#tomerge → 🔗antiticks
* https://www.mosquitomagnet.com/articles/10-scents-that-repel-mosquitoes
* some edible herbs on window sills
* window or bed nets
Treating:
* do not scratch!
* any kind of cream helps:
aloe & calendula works
Maps:
https://www.ecdc.europa.eu/en/disease-vectors/surveillance-and-disease-data/mosquito-maps
Repelling:
* Similar to ticks:
#tomerge → 🔗antiticks
* https://www.mosquitomagnet.com/articles/10-scents-that-repel-mosquitoes
* some edible herbs on window sills
* window or bed nets
Treating:
* do not scratch!
* any kind of cream helps:
aloe & calendula works
Maps:
https://www.ecdc.europa.eu/en/disease-vectors/surveillance-and-disease-data/mosquito-maps
¶ (species recognition)
https://www.mosquitomagnet.com/articles/how-big-can-mosquitoes-get
sizes
https://www.ecdc.europa.eu/en/publications-data/aedes-albopictus-current-known-distribution-europe-april-2017
EU map
https://twitter.com/ECDC_Outbreaks/status/1031541871192014848/photo/1
the 4 main species
https://www.mosquitomagnet.com/articles/how-big-can-mosquitoes-get
sizes
https://www.ecdc.europa.eu/en/publications-data/aedes-albopictus-current-known-distribution-europe-april-2017
EU map
https://twitter.com/ECDC_Outbreaks/status/1031541871192014848/photo/1
the 4 main species
¶ (in Canarias)
https://archive.org/stream/cbarchive_118779_notesonthemosquitofaunaoftheca1980/MS_V12_N3_P349-355_djvu.txt
notes on mosquito fauna in Fuerteventura (1980)
"""
The Culicidae fauna of the Canary Islands comprises a total of 11 species
ABSTRACT. The Culicidae fauna of the Canary Islands comprises a total of 11
species: Aedes (Ooh.) oaspius (Pallas), Aedes (Fin.) eatoni (Edwards),
Anopheles (Cel.) hispaniola (Theobald), Anopheles (Cel.) multicolor Cambouliu,
Anopheles (Cel.) sevgentii (Theobald), Culiseta (All.) longiaveolata (Macquart),
Culex (Mai.) avbieeni Salem, Culex (Mai.) hortensis Ficalbi, Culex (Cux.)
latioinctus Edwards, Culex (Cux.) pipiens Linn., and Culex (Cux.) theileri
Theobald.
The records for two species are considered to be doubtful, namely, Aedes
(Ooh.) detritus (Haliday) and Culiseta (Cus.) annulata (Schrank), ^\\^^e Aedes
(Stg.) aegypti (L.) has been eradicated.
"""
BOLD = marked for Lanza/Fuerte
https://archive.org/stream/cbarchive_118779_notesonthemosquitofaunaoftheca1980/MS_V12_N3_P349-355_djvu.txt
notes on mosquito fauna in Fuerteventura (1980)
"""
The Culicidae fauna of the Canary Islands comprises a total of 11 species
ABSTRACT. The Culicidae fauna of the Canary Islands comprises a total of 11
species: Aedes (Ooh.) oaspius (Pallas), Aedes (Fin.) eatoni (Edwards),
Anopheles (Cel.) hispaniola (Theobald), Anopheles (Cel.) multicolor Cambouliu,
Anopheles (Cel.) sevgentii (Theobald), Culiseta (All.) longiaveolata (Macquart),
Culex (Mai.) avbieeni Salem, Culex (Mai.) hortensis Ficalbi, Culex (Cux.)
latioinctus Edwards, Culex (Cux.) pipiens Linn., and Culex (Cux.) theileri
Theobald.
The records for two species are considered to be doubtful, namely, Aedes
(Ooh.) detritus (Haliday) and Culiseta (Cus.) annulata (Schrank), ^\\^^e Aedes
(Stg.) aegypti (L.) has been eradicated.
"""
BOLD = marked for Lanza/Fuerte
¶ Culex pipiens ("common house mosquito")
https://en.wikipedia.org/wiki/Culex_pipiens
Spreads:
west nile fever
https://en.wikipedia.org/wiki/Culex_pipiens
Spreads:
west nile fever
¶ Aedes aegypti ("yellow fever mosquito")
brought to Fuerteventura : 2018-2019
supposedly eradicated !
recognize:
black+white stripes
_________________________
transmits:
* zika
* yellow fever
* dengue !
https://funccet.es/en/se-confirma-la-erradicacion-del-mosquito-aedes-aegypti-de-fuerteventura/
erradicated ?
sources:
* https://www.cleaningcommunity.net/fuerteventura-health-chefs-step-up-action-against-aedes-aegypti/ !!!
* https://www.ecdc.europa.eu/en/news-events/new-settlements-aedes-aegypti-raising-concerns-continental-eu
* http://www.cresa.cat/blogs/sociedad/en/aedes-aegypti-detectat-a-fuerteventura-illes-canaries/
* [...]
...also:
* https://www.researchgate.net/publication/322208539_Identificacion_del_mosquito_Aedes_aegypti_en_Fuerteventura_Evaluacion_rapida_de_riesgo
* [...]
"""
The importance of citizens partecipation is also being stressed and if anyone spots what they think is one of the mosquitos, they are being urged to send details and even photos to the health department or through the app Mosquito Alert mobile app.
They can also send photos of stings that they consider suspicious because of the strong inflammatory reaction accompanied by great stinging.
Whenever photos of specimen or suspicious bites are sent, it is essential to clearly indicate the geographical area where the mosquito was detected or the suspicious bite occurred.
"""
brought to Fuerteventura : 2018-2019
supposedly eradicated !
recognize:
black+white stripes
_________________________
transmits:
* zika
* yellow fever
* dengue !
https://funccet.es/en/se-confirma-la-erradicacion-del-mosquito-aedes-aegypti-de-fuerteventura/
erradicated ?
sources:
* https://www.cleaningcommunity.net/fuerteventura-health-chefs-step-up-action-against-aedes-aegypti/ !!!
* https://www.ecdc.europa.eu/en/news-events/new-settlements-aedes-aegypti-raising-concerns-continental-eu
* http://www.cresa.cat/blogs/sociedad/en/aedes-aegypti-detectat-a-fuerteventura-illes-canaries/
* [...]
...also:
* https://www.researchgate.net/publication/322208539_Identificacion_del_mosquito_Aedes_aegypti_en_Fuerteventura_Evaluacion_rapida_de_riesgo
* [...]
"""
The importance of citizens partecipation is also being stressed and if anyone spots what they think is one of the mosquitos, they are being urged to send details and even photos to the health department or through the app Mosquito Alert mobile app.
They can also send photos of stings that they consider suspicious because of the strong inflammatory reaction accompanied by great stinging.
Whenever photos of specimen or suspicious bites are sent, it is essential to clearly indicate the geographical area where the mosquito was detected or the suspicious bite occurred.
"""
¶ Aedes albopictus ("tiger mosquito")
https://www.ecdc.europa.eu/en/disease-vectors/facts/mosquito-factsheets/aedes-albopictus
"""
This mosquito species is a known vector of chikungunya virus, dengue virus and dirofilariasis.
"""
https://www.ecdc.europa.eu/en/disease-vectors/facts/mosquito-factsheets/aedes-albopictus
"""
This mosquito species is a known vector of chikungunya virus, dengue virus and dirofilariasis.
"""
¶ Anopheles
https://upload.wikimedia.org/wikipedia/commons/a/ad/Anopheles-range-map.png
map
https://en.wikipedia.org/wiki/Anopheles_gambiae
"most well known", for being the main Malaria vector
https://www.ecdc.europa.eu/en/disease-vectors/facts/mosquito-factsheets/anopheles-atroparvus
"""
Adults of Anopheles atroparvus are almost impossible to distinguish from other sibling species of the Anopheles maculipennis complex and are most easily identified morphologically by examining their eggs
"""
transmits:
* malaria:
https://www.ecdc.europa.eu/en/disease-vectors/facts/mosquito-factsheets/anopheles-labranchiae
* elephantiasis:
"""The An. gambiae mosquito additionally transmits Wuchereria bancrofti which causes Lymphatic philariasis, more commonly known as elephantiasis"""
ID:
"""The mechanism of species recognition appears to be sounds emitted by the wings and identified by Johnston's organ.[10]"""
-----------------------------------------------------
!!! #project #mobile.server
constant environment sound-ID
https://upload.wikimedia.org/wikipedia/commons/a/ad/Anopheles-range-map.png
map
https://en.wikipedia.org/wiki/Anopheles_gambiae
"most well known", for being the main Malaria vector
https://www.ecdc.europa.eu/en/disease-vectors/facts/mosquito-factsheets/anopheles-atroparvus
"""
Adults of Anopheles atroparvus are almost impossible to distinguish from other sibling species of the Anopheles maculipennis complex and are most easily identified morphologically by examining their eggs
"""
transmits:
* malaria:
https://www.ecdc.europa.eu/en/disease-vectors/facts/mosquito-factsheets/anopheles-labranchiae
* elephantiasis:
"""The An. gambiae mosquito additionally transmits Wuchereria bancrofti which causes Lymphatic philariasis, more commonly known as elephantiasis"""
ID:
"""The mechanism of species recognition appears to be sounds emitted by the wings and identified by Johnston's organ.[10]"""
-----------------------------------------------------
!!! #project #mobile.server
constant environment sound-ID
¶ Anopheles → Plasmodium falciparum→ malaria
"""
Some mosquitoes carry this parasite, which causes malaria. The disease kills more people than any other of its kind. It feels like the flu, and it causes body chills, fever, and sometimes nausea or vomiting. A doctor has to look at someone's blood under a microscope to tell if they have it. Early treatment is best. Certain prescription drugs can cure most types.
"""
https://en.wikipedia.org/wiki/Malaria
"""
Some mosquitoes carry this parasite, which causes malaria. The disease kills more people than any other of its kind. It feels like the flu, and it causes body chills, fever, and sometimes nausea or vomiting. A doctor has to look at someone's blood under a microscope to tell if they have it. Early treatment is best. Certain prescription drugs can cure most types.
"""
https://en.wikipedia.org/wiki/Malaria
¶ mosquitos → chikungunya virus
http://www.cresa.cat/blogs/sociedad/en/que-hi-fa-el-virus-de-chikungunya-a-catalunya/
"""
In 2006, around 38% of the population of the French island La Reunion was infected. Unusually, during this epidemic, few asymptomatic infections and a relatively high mortality rate were observed, most likely due to the lack of prior population immunity. Fears have grown for outbreaks of CHIKV and other arboviral diseases in America and Europe following identification of the Asian tiger mosquito (Aedes albopictus) as the major vector.
The first transmission within continental Europe was reported from north-eastern Italy in August 2007. Every year, imported cases among tourists are identified in several European countries. An outbreak of Chikungunya in the Caribbean region was reported from the French part of the island of Saint Martin on 6 December 2013. Since then, autochthonous transmission of chikungunya has been reported from several islands in the Caribbean and recently for the first time in South America (French Guiana). More recently, three cases of infection with Chikungunya virus have been detected in Catalonia in eight persons who had recently traveled to Caribbean countries where the disease is endemic.
"""
https://en.wikipedia.org/wiki/Chikungunya
"""
Chikungunya is an infection caused by the Chikungunya virus (CHIKV).[5][3] Symptoms include fever and joint pains.[2] These typically occur two to twelve days after exposure.[3] Other symptoms may include headache, muscle pain, joint swelling, and a rash.[2] Symptoms usually improve within a week; however, occasionally the joint pain may last for months or years.[2][6] The risk of death is around 1 in 1,000.[4] The very young, old, and those with other health problems are at risk of more severe disease.[2]
The virus is spread between people by two types of mosquitos: Aedes albopictus and Aedes aegypti.[3] They mainly bite during the day.[7] The virus may circulate within a number of animals including birds and rodents.[3] Diagnosis is by either testing the blood for the virus's RNA or antibodies to the virus.[3] The symptoms can be mistaken for those of dengue fever and Zika fever.[3] It is believed most people become immune after a single infection.[2]
[...]
Around 85% of people infected with Chikungunya virus experience symptoms, typically beginning with a sudden high fever above 39 °C (102 °F).[10] The fever is soon followed by severe muscle and joint pain.[11] Pain usually affects multiple joints in the arms and legs, and is symmetric – i.e. if one elbow is affected, the other is as well
[...]
Many people continue to have symptoms after the "acute phase" resolves, termed the "post-acute phase" for symptoms lasting three weeks to three months, and the "chronic stage" for symptoms lasting longer than three months.[11] In both cases, the lasting symptoms tend to be joint pains: arthritis, tenosynovitis, and/or bursitis.[11] If the affected person had pre-existing joint issues, these tend to worsen.[11] Overuse of a joint can result in painful swelling, stiffness, nerve damage, and neuropathic pain.[11] Typically the joint pain improves with time; however, the chronic stage can last anywhere from a few months to several years
"""
______
20231010: Discovered in Trieste (Italy/Slovenia)
https://www.rtvslo.si/zdravje/v-trstu-prvi-primer-tropske-cikungunje-ki-jo-sirijo-tigrasti-komarji/684407
http://www.cresa.cat/blogs/sociedad/en/que-hi-fa-el-virus-de-chikungunya-a-catalunya/
"""
In 2006, around 38% of the population of the French island La Reunion was infected. Unusually, during this epidemic, few asymptomatic infections and a relatively high mortality rate were observed, most likely due to the lack of prior population immunity. Fears have grown for outbreaks of CHIKV and other arboviral diseases in America and Europe following identification of the Asian tiger mosquito (Aedes albopictus) as the major vector.
The first transmission within continental Europe was reported from north-eastern Italy in August 2007. Every year, imported cases among tourists are identified in several European countries. An outbreak of Chikungunya in the Caribbean region was reported from the French part of the island of Saint Martin on 6 December 2013. Since then, autochthonous transmission of chikungunya has been reported from several islands in the Caribbean and recently for the first time in South America (French Guiana). More recently, three cases of infection with Chikungunya virus have been detected in Catalonia in eight persons who had recently traveled to Caribbean countries where the disease is endemic.
"""
https://en.wikipedia.org/wiki/Chikungunya
"""
Chikungunya is an infection caused by the Chikungunya virus (CHIKV).[5][3] Symptoms include fever and joint pains.[2] These typically occur two to twelve days after exposure.[3] Other symptoms may include headache, muscle pain, joint swelling, and a rash.[2] Symptoms usually improve within a week; however, occasionally the joint pain may last for months or years.[2][6] The risk of death is around 1 in 1,000.[4] The very young, old, and those with other health problems are at risk of more severe disease.[2]
The virus is spread between people by two types of mosquitos: Aedes albopictus and Aedes aegypti.[3] They mainly bite during the day.[7] The virus may circulate within a number of animals including birds and rodents.[3] Diagnosis is by either testing the blood for the virus's RNA or antibodies to the virus.[3] The symptoms can be mistaken for those of dengue fever and Zika fever.[3] It is believed most people become immune after a single infection.[2]
[...]
Around 85% of people infected with Chikungunya virus experience symptoms, typically beginning with a sudden high fever above 39 °C (102 °F).[10] The fever is soon followed by severe muscle and joint pain.[11] Pain usually affects multiple joints in the arms and legs, and is symmetric – i.e. if one elbow is affected, the other is as well
[...]
Many people continue to have symptoms after the "acute phase" resolves, termed the "post-acute phase" for symptoms lasting three weeks to three months, and the "chronic stage" for symptoms lasting longer than three months.[11] In both cases, the lasting symptoms tend to be joint pains: arthritis, tenosynovitis, and/or bursitis.[11] If the affected person had pre-existing joint issues, these tend to worsen.[11] Overuse of a joint can result in painful swelling, stiffness, nerve damage, and neuropathic pain.[11] Typically the joint pain improves with time; however, the chronic stage can last anywhere from a few months to several years
"""
______
20231010: Discovered in Trieste (Italy/Slovenia)
https://www.rtvslo.si/zdravje/v-trstu-prvi-primer-tropske-cikungunje-ki-jo-sirijo-tigrasti-komarji/684407
¶ Psorophora ciliata (massive)
https://en.wikipedia.org/wiki/Psorophora_ciliata
"""
Not only are these mosquitoes aggressive towards humans and other animals as adults, but P. ciliata larvae are known for preying on other mosquito species' larvae and even tadpoles.[1] Campos, Fernandez, and Sy found in their 2004 study that P. ciliata were frequent predators to the mosquito species Ochlerotatus albifasciatus in Buenos Aires, Argentina and impact the populations of O. albifasciatus.[5] Females are aggressive, preferring to feed on large mammals,[2] and are most active during spring and summer in woodlands or fields during the day or night.[3] They lay eggs either as single eggs on moist soil, or as an egg raft on top of ephemeral pools of water. Typically, females in the genus are capable of laying their eggs on dry or damp land to hatch months or years later, depending on the species.[4]
"""
https://en.wikipedia.org/wiki/Psorophora_ciliata
"""
Not only are these mosquitoes aggressive towards humans and other animals as adults, but P. ciliata larvae are known for preying on other mosquito species' larvae and even tadpoles.[1] Campos, Fernandez, and Sy found in their 2004 study that P. ciliata were frequent predators to the mosquito species Ochlerotatus albifasciatus in Buenos Aires, Argentina and impact the populations of O. albifasciatus.[5] Females are aggressive, preferring to feed on large mammals,[2] and are most active during spring and summer in woodlands or fields during the day or night.[3] They lay eggs either as single eggs on moist soil, or as an egg raft on top of ephemeral pools of water. Typically, females in the genus are capable of laying their eggs on dry or damp land to hatch months or years later, depending on the species.[4]
"""
¶FLIES
* flies do not grow in size! smaller / bigger flies are just different species.
* can lay eggs into infested wounds
general:
* https://www.healthline.com/health/fly-bites#pictures
* http://www.idph.state.il.us/envhealth/pcbitingflies.htm
* [...]
* flies do not grow in size! smaller / bigger flies are just different species.
* can lay eggs into infested wounds
general:
* https://www.healthline.com/health/fly-bites#pictures
* http://www.idph.state.il.us/envhealth/pcbitingflies.htm
* [...]
¶ Black flies (Simuliidae)
https://en.wikipedia.org/wiki/Black_fly
https://extension.unh.edu/resource/black-flies-fact-sheet
"is any member of the family Simuliidae of the Culicomorpha infraorder"
Bite for blood during daylight:
"""They are usually small, black or gray, with short legs, and antennae. They are a common nuisance for humans, and many U.S. states have programs to suppress the black fly population
[...]
Only four genera in the family Simuliidae, Simulium, Prosimulium, Austrosimulium, and Cnephia, contain species that feed on people, though other species prefer to feed on other mammals or on birds. Simulium, the type genus, is the most widespread and is a vector for several diseases, including river blindness.
[...]
Biting flies feed during daylight hours only and
tend to zero in on areas of thinner skin, such as the nape of the neck or ears and ankles.
"""
Transmits:
"""
They spread several diseases, including river blindness in Africa (Simulium damnosum and S. neavei) and the Americas (S. callidum and S. metallicum in Central America, S. ochraceum in Central and South America).
"""
_____________________
... is this biting behind the ears???
###
https://en.wikipedia.org/wiki/Black_fly
https://extension.unh.edu/resource/black-flies-fact-sheet
"is any member of the family Simuliidae of the Culicomorpha infraorder"
Bite for blood during daylight:
"""They are usually small, black or gray, with short legs, and antennae. They are a common nuisance for humans, and many U.S. states have programs to suppress the black fly population
[...]
Only four genera in the family Simuliidae, Simulium, Prosimulium, Austrosimulium, and Cnephia, contain species that feed on people, though other species prefer to feed on other mammals or on birds. Simulium, the type genus, is the most widespread and is a vector for several diseases, including river blindness.
[...]
Biting flies feed during daylight hours only and
tend to zero in on areas of thinner skin, such as the nape of the neck or ears and ankles.
"""
Transmits:
"""
They spread several diseases, including river blindness in Africa (Simulium damnosum and S. neavei) and the Americas (S. callidum and S. metallicum in Central America, S. ochraceum in Central and South America).
"""
_____________________
... is this biting behind the ears???
¶ Blandford fly (Simulium posticatum)
https://en.wikipedia.org/wiki/Blandford_fly
https://alchetron.com/Blandford-fly
https://en.wikipedia.org/wiki/Blandford_fly
https://alchetron.com/Blandford-fly
¶ Biting Midges (GNATS #1)
Diptera
https://en.wikipedia.org/wiki/Ceratopogonidae
Ceratopogonidae is a family of flies commonly known as no-see-ums, or biting midges, generally 1–3 mm in length. The family includes more than 5,000 species,[1] distributed worldwide, apart from the Antarctic and the Arctic.
merge in !!!
_____________
https://en.wikipedia.org/wiki/Culicoides_imicola
[...]
________
https://parasitesandvectors.biomedcentral.com/articles/10.1186/1756-3305-5-147 !!!
"""
Culicoides (Diptera: Ceratopogonidae) biting midges are vectors for a diversity of pathogens including bluetongue virus (BTV) that generate important economic losses. BTV has expanded its range in recent decades, probably due to the expansion of its main vector and the presence of other autochthonous competent vectors. Although the Canary Islands are still free of bluetongue disease (BTD), Spain and Europe have had to face up to a spread of bluetongue with disastrous consequences
"""
Bluetonge virus:
"""Bluetongue disease is a noncontagious, insect-borne, viral disease of ruminants, mainly sheep and less frequently cattle,[1] goats, buffalo, deer, dromedaries, and antelope. It is caused by Bluetongue virus (BTV). The virus is transmitted by the midges Culicoides imicola, Culicoides variipennis, and other culicoids."""
https://www.google.com/search?q=Biting+midges&client=ubuntu&hs=aQg&channel=fs&source=lnms&tbm=isch&sa=X&ved=2ahUKEwii0arkp_3nAhVHQBoKHVszDlIQ_AUoAXoECBgQAw&biw=1138&bih=520&dpr=1.2#imgrc=lt6qlXO5NTF7wM
Photos !
Diptera
https://en.wikipedia.org/wiki/Ceratopogonidae
Ceratopogonidae is a family of flies commonly known as no-see-ums, or biting midges, generally 1–3 mm in length. The family includes more than 5,000 species,[1] distributed worldwide, apart from the Antarctic and the Arctic.
merge in !!!
_____________
https://en.wikipedia.org/wiki/Culicoides_imicola
[...]
________
https://parasitesandvectors.biomedcentral.com/articles/10.1186/1756-3305-5-147 !!!
"""
Culicoides (Diptera: Ceratopogonidae) biting midges are vectors for a diversity of pathogens including bluetongue virus (BTV) that generate important economic losses. BTV has expanded its range in recent decades, probably due to the expansion of its main vector and the presence of other autochthonous competent vectors. Although the Canary Islands are still free of bluetongue disease (BTD), Spain and Europe have had to face up to a spread of bluetongue with disastrous consequences
"""
Bluetonge virus:
"""Bluetongue disease is a noncontagious, insect-borne, viral disease of ruminants, mainly sheep and less frequently cattle,[1] goats, buffalo, deer, dromedaries, and antelope. It is caused by Bluetongue virus (BTV). The virus is transmitted by the midges Culicoides imicola, Culicoides variipennis, and other culicoids."""
https://www.google.com/search?q=Biting+midges&client=ubuntu&hs=aQg&channel=fs&source=lnms&tbm=isch&sa=X&ved=2ahUKEwii0arkp_3nAhVHQBoKHVszDlIQ_AUoAXoECBgQAw&biw=1138&bih=520&dpr=1.2#imgrc=lt6qlXO5NTF7wM
Photos !
¶ Horse flies / Deer flies
https://en.wikipedia.org/wiki/Horse-fly
https://en.wikipedia.org/wiki/Tabanus_bovinus (biggest in Croatia)
https://en.wikipedia.org/wiki/Horse-fly
https://en.wikipedia.org/wiki/Tabanus_bovinus (biggest in Croatia)
¶ Tse-Tse fly → Trypanosomiasis
glossina
https://es.wikipedia.org/wiki/Glossina
https://faculty.ucr.edu/~legneref/medical/trypanosomiasis.htm
"""
What are the signs and symptoms of East African trypanosomiasis? A bite by the tsetse fly is often painful and can develop into a red sore, also called a chancre. Fever, severe headaches, irritability, extreme fatigue, swollen lymph nodes, and aching muscles and joints are common symptoms of sleeping sickness.
"""
__________
merge in !!!
__________
https://en.wikipedia.org/wiki/Tsetse_fly
https://www.tripsavvy.com/avoiding-the-tsetse-fly-on-safari-1454081
https://www.cdc.gov/parasites/sleepingsickness/gen_info/faqs-east.html
https://www.iaea.org/newscenter/news/tsetse-free-for-20-years-thanks-to-a-nuclear-technique-the-island-of-unguja-zanzibar
destroying with irradiation + release
https://www.npr.org/sections/goatsandsoda/2015/08/04/427181595/in-the-fight-against-tsetse-flies-blue-is-the-new-black
what. they love blue !
"""The blue material catches the flies' interest. As the tsetses circle the blue cloth, mesmerized, they hit the poisoned netting, which they can't see. The insecticide kills them within three minutes."""
glossina
https://es.wikipedia.org/wiki/Glossina
https://faculty.ucr.edu/~legneref/medical/trypanosomiasis.htm
"""
What are the signs and symptoms of East African trypanosomiasis? A bite by the tsetse fly is often painful and can develop into a red sore, also called a chancre. Fever, severe headaches, irritability, extreme fatigue, swollen lymph nodes, and aching muscles and joints are common symptoms of sleeping sickness.
"""
__________
merge in !!!
__________
https://en.wikipedia.org/wiki/Tsetse_fly
https://www.tripsavvy.com/avoiding-the-tsetse-fly-on-safari-1454081
https://www.cdc.gov/parasites/sleepingsickness/gen_info/faqs-east.html
https://www.iaea.org/newscenter/news/tsetse-free-for-20-years-thanks-to-a-nuclear-technique-the-island-of-unguja-zanzibar
destroying with irradiation + release
https://www.npr.org/sections/goatsandsoda/2015/08/04/427181595/in-the-fight-against-tsetse-flies-blue-is-the-new-black
what. they love blue !
"""The blue material catches the flies' interest. As the tsetses circle the blue cloth, mesmerized, they hit the poisoned netting, which they can't see. The insecticide kills them within three minutes."""
¶ Sand flies (GNATS #2)
https://en.wikipedia.org/wiki/Sandfly
Totally confused vocabulary:
"""
In the United States, sandfly may refer to certain horse flies that are also known as "greenheads" (family Tabanidae), or to members of the family Ceratopogonidae. Outside the United States, sandfly may refer to members of the subfamily Phlebotominae within the Psychodidae. Biting midges (Ceratopogonidae) are sometimes called sandflies or no-see-ums (no-see-em, noseeum). New Zealand sandflies are in the genus Austrosimulium, a type of black fly.[1]
"""
____________
merge in !!!
____________
https://www.ncbi.nlm.nih.gov/pubmed/28048977
g: "sandfly canary islands"
"Among the viruses that sandflies can carry is the Chandipura virus, which, as a cousin of rabies, is very deadly. There was an outbreak in India in 2010. "
_____________________________
https://en.wikipedia.org/wiki/Leishmaniasis
ewwwww
https://www.researchgate.net/publication/312056031_Phlebotomine_sandflies_Diptera_Phlebotomidae_of_Lanzarote_Island_Canary_Islands_Spain_Ecological_survey_and_evaluation_of_the_risk_of_Leishmania_transmission
leishmania in lanzarote ?!
"""
No specimen of the Phlebotomus genus was captured and given that none of the species captured has been demonstrated vectors of human pathogenic Leishmania and considering that they were captured in low frequency and density, it can be concluded that the current leishmaniasis transmission risk is null.
"""
OK good.
https://en.wikipedia.org/wiki/Sandfly
Totally confused vocabulary:
"""
In the United States, sandfly may refer to certain horse flies that are also known as "greenheads" (family Tabanidae), or to members of the family Ceratopogonidae. Outside the United States, sandfly may refer to members of the subfamily Phlebotominae within the Psychodidae. Biting midges (Ceratopogonidae) are sometimes called sandflies or no-see-ums (no-see-em, noseeum). New Zealand sandflies are in the genus Austrosimulium, a type of black fly.[1]
"""
____________
merge in !!!
____________
https://www.ncbi.nlm.nih.gov/pubmed/28048977
g: "sandfly canary islands"
"Among the viruses that sandflies can carry is the Chandipura virus, which, as a cousin of rabies, is very deadly. There was an outbreak in India in 2010. "
_____________________________
https://en.wikipedia.org/wiki/Leishmaniasis
ewwwww
https://www.researchgate.net/publication/312056031_Phlebotomine_sandflies_Diptera_Phlebotomidae_of_Lanzarote_Island_Canary_Islands_Spain_Ecological_survey_and_evaluation_of_the_risk_of_Leishmania_transmission
leishmania in lanzarote ?!
"""
No specimen of the Phlebotomus genus was captured and given that none of the species captured has been demonstrated vectors of human pathogenic Leishmania and considering that they were captured in low frequency and density, it can be concluded that the current leishmaniasis transmission risk is null.
"""
OK good.
¶ flies → mites (vector)
see:
* https://bugguide.net/node/view/16764
* CHT microscopy ~ 2020/04
???:
* how to ID the mites
* how to do it at scale? (#monitoring)
* [...]
see:
* https://bugguide.net/node/view/16764
* CHT microscopy ~ 2020/04
???:
* how to ID the mites
* how to do it at scale? (#monitoring)
* [...]
¶ (more/unsorted)
https://images-prod.healthline.com/hlcmsresource/images/Image-Galleries/Fly-Bites/642x361_Slide_4_Fly_bites.jpg
nice neck bites
ewww
tse tse ?
https://images-prod.healthline.com/hlcmsresource/images/Image-Galleries/Fly-Bites/642x361_Slide_4_Fly_bites.jpg
nice neck bites
ewww
tse tse ?
¶ (Flies in Fuerteventura)
https://www.tripadvisor.com/ShowTopic-g187467-i272-k9006240-Flies-Fuerteventura_Canary_Islands.html
"""Most of them don't actually bite - just one or two types that do, but that doesn't help much if you've got some biters round you."""
https://www.tripadvisor.com/ShowTopic-g187467-i272-k9006240-Flies-Fuerteventura_Canary_Islands.html
"""Most of them don't actually bite - just one or two types that do, but that doesn't help much if you've got some biters round you."""
¶ OBSERVED: Sand fly? Tse tse fly?
Got 3, made good microscope photos from today (2020/04/11).
Looks a bit like this but not?
https://www.iaea.org/sites/default/files/styles/original_image_size/public/tsetsefly.jpg?itok=CyUtGZli
Circles around me, but does not really seem to land?
###
Got 3, made good microscope photos from today (2020/04/11).
Looks a bit like this but not?
https://www.iaea.org/sites/default/files/styles/original_image_size/public/tsetsefly.jpg?itok=CyUtGZli
Circles around me, but does not really seem to land?
###
¶ (general "Dermatophytosis")
esp: "Dermatofitosis / tiñas"
slo: "Glivične kožne bolezni / kožne mikoze"
_____________________
https://en.wikipedia.org/wiki/Dermatophytosis
Dermatophytosis, also known as ringworm,
"""
Dermatophytosis, also known as ringworm, is a fungal infection of the skin.[2] Typically it results in a red, itchy, scaly, circular rash.[1] Hair loss may occur in the area affected.[1] Symptoms begin four to fourteen days after exposure.[1] Multiple areas can be affected at a given time.[4]
About 40 types of fungi can cause ringworm.[2] They are typically of the Trichophyton, Microsporum, or Epidermophyton type.[2]
"""
____________________
Trending:
"Are among the most common skin diseases and are becoming ever more common because of growing use of wide-spectrum antibiotics."
via https://sl.wikipedia.org/wiki/Glivi%C4%8Dne_ko%C5%BEne_bolezni (SLO)
Highly contagious:
* skin-to-skin contact
* sharing towels:
(and ... people washing towels at 40°C ...)
* [...]
esp: "Dermatofitosis / tiñas"
slo: "Glivične kožne bolezni / kožne mikoze"
_____________________
https://en.wikipedia.org/wiki/Dermatophytosis
Dermatophytosis, also known as ringworm,
"""
Dermatophytosis, also known as ringworm, is a fungal infection of the skin.[2] Typically it results in a red, itchy, scaly, circular rash.[1] Hair loss may occur in the area affected.[1] Symptoms begin four to fourteen days after exposure.[1] Multiple areas can be affected at a given time.[4]
About 40 types of fungi can cause ringworm.[2] They are typically of the Trichophyton, Microsporum, or Epidermophyton type.[2]
"""
____________________
Trending:
"Are among the most common skin diseases and are becoming ever more common because of growing use of wide-spectrum antibiotics."
via https://sl.wikipedia.org/wiki/Glivi%C4%8Dne_ko%C5%BEne_bolezni (SLO)
Highly contagious:
* skin-to-skin contact
* sharing towels:
(and ... people washing towels at 40°C ...)
* [...]
¶ dermatophytes → "ringworm"/"tinea"
"""
Dermatophytes produce an infection commonly known as ringworm or tinea. It can appear as "jock itch" in the groin or inner thighs (tinea cruris); on the scalp and hair (tinea capitis) resulting in brittle hair shafts that fall out easily.
Tinea unguium affects the nails and athlete's foot (tinea pedis) affects the feet.
Tinea versicolor refers to a fungal infection of the skin caused by Malassezia furfur. It appears anywhere on the skin and produces red or gray, scaly patches of itchy skin. Deeper infections may be discoloured, ulcerative and purulent.
"""
https://en.wikipedia.org/wiki/Tinea_versicolor
(==spotted skin)
via https://en.wikipedia.org/wiki/Malassezia_furfur
"""
It is associated with a variety of dermatological conditions caused by fungal infections, notably seborrhoeic dermatitis and tinea versicolor. As an opportunistic pathogen, it has further been associated with dandruff, malassezia folliculitis, pityriasis versicolor (alba), and malassezia intertrigo,[1] as well as catheter-related fungemia and pneumonia in patients receiving hematopoietic transplants. The fungus can also affect other animals, including dogs.
"""
https://en.wikipedia.org/wiki/Onychomycosis
"""
Onychomycosis, also known as tinea unguium,[4] is a fungal infection of the nail.[2] Symptoms may include white or yellow nail discoloration, thickening of the nail, and separation of the nail from the nail bed.[2][3] Toenails or fingernails may be affected, but it is more common for toenails
[...]
Onychomycosis occurs in about 10 percent of the adult population,[2] with older people more frequently affected.[2] Males are affected more often than females.
[...]
Dermatophytids are fungus-free skin lesions that sometimes form as a result of a fungus infection in another part of the body. This could take the form of a rash or itch in an area of the body that is not infected with the fungus. Dermatophytids can be thought of as an allergic reaction to the fungus.
[...]
Tea tree oil is not recommended as a treatment, since it is not effective and can irritate the surrounding skin.[35]
"""
"""
Dermatophytes produce an infection commonly known as ringworm or tinea. It can appear as "jock itch" in the groin or inner thighs (tinea cruris); on the scalp and hair (tinea capitis) resulting in brittle hair shafts that fall out easily.
Tinea unguium affects the nails and athlete's foot (tinea pedis) affects the feet.
Tinea versicolor refers to a fungal infection of the skin caused by Malassezia furfur. It appears anywhere on the skin and produces red or gray, scaly patches of itchy skin. Deeper infections may be discoloured, ulcerative and purulent.
"""
https://en.wikipedia.org/wiki/Tinea_versicolor
(==spotted skin)
via https://en.wikipedia.org/wiki/Malassezia_furfur
"""
It is associated with a variety of dermatological conditions caused by fungal infections, notably seborrhoeic dermatitis and tinea versicolor. As an opportunistic pathogen, it has further been associated with dandruff, malassezia folliculitis, pityriasis versicolor (alba), and malassezia intertrigo,[1] as well as catheter-related fungemia and pneumonia in patients receiving hematopoietic transplants. The fungus can also affect other animals, including dogs.
"""
https://en.wikipedia.org/wiki/Onychomycosis
"""
Onychomycosis, also known as tinea unguium,[4] is a fungal infection of the nail.[2] Symptoms may include white or yellow nail discoloration, thickening of the nail, and separation of the nail from the nail bed.[2][3] Toenails or fingernails may be affected, but it is more common for toenails
[...]
Onychomycosis occurs in about 10 percent of the adult population,[2] with older people more frequently affected.[2] Males are affected more often than females.
[...]
Dermatophytids are fungus-free skin lesions that sometimes form as a result of a fungus infection in another part of the body. This could take the form of a rash or itch in an area of the body that is not infected with the fungus. Dermatophytids can be thought of as an allergic reaction to the fungus.
[...]
Tea tree oil is not recommended as a treatment, since it is not effective and can irritate the surrounding skin.[35]
"""
¶ (general treatment)
#medical
* apple cider vinegar (strong antifungal properties)
"""
Topical application of antifungal medications such as azole antimycotics, ciclopirox olamine, piroctone-olamine, zinc pyrithione, or sulfur compounds are commonly prescribed to treat diseases caused by Malassezia furfur.[5]
"""
"""
Research suggests that fungi are sensitive to heat, typically 40–60 °C (104–140 °F). The basis of laser treatment is to try to heat the nail bed to these temperatures in order to disrupt fungal growth.[42] As of 2013 research into laser treatment seems promising.[2] There is also ongoing development in photodynamic therapy, which uses laser or LED light to activate photosensitisers that eradicate fungi.[43]
"""
* apple cider vinegar (strong antifungal properties)
"""
Topical application of antifungal medications such as azole antimycotics, ciclopirox olamine, piroctone-olamine, zinc pyrithione, or sulfur compounds are commonly prescribed to treat diseases caused by Malassezia furfur.[5]
"""
"""
Research suggests that fungi are sensitive to heat, typically 40–60 °C (104–140 °F). The basis of laser treatment is to try to heat the nail bed to these temperatures in order to disrupt fungal growth.[42] As of 2013 research into laser treatment seems promising.[2] There is also ongoing development in photodynamic therapy, which uses laser or LED light to activate photosensitisers that eradicate fungi.[43]
"""
¶ cats/dogs → microsporum → microsporosis
(SLO): https://sl.wikipedia.org/wiki/Mikrosporija / mikrosporoza
(DE): https://de.wikipedia.org/wiki/Mikrosporie
Many can be gotten from pets, like Microspirosis
"""
Bolezen pogosto povzroča Microsporum canis in se na ljudi po navadi prenese z mačk, redkeje s psov. Redkejša povzročitelja mokrosporije sta M. gypseum (zoofilni dermatofit) in M. audouinii (antropofilni dermatofit). Vir okužbe so najpogosteje živali v okolici, obolevajo zlasti šolski otroci. Pogostejša je pri ženskem spolu ter od julija do oktobra.
"""
http://iloveanimalfriends.over-blog.com/2015/10/microsporosis-in-your-pets.html
"""
Microsporosis in the cats (less frequently in dogs) manifests in one or more areas of alopecia or without hair on the animal's body. These changes to the skin can be substantially round, oval or irregularly shaped.
[...]
There are two forms Microsporosis in humans, depending on the location:
If the infected scalp hair in these places waste in circles or oval surfaces and has a height of two to four millimeters above the skin.
In the case of contamination of other parts of the body there are changes in the skin in the form of circles with a raised edge in red, while the interior of the circle normal color (in the image). Also, there is also fine scaling in the middle rounds as possible are less crusting. Changes may be accompanied by moderate or intense itching.
"""
______________
https://en.wikipedia.org/wiki/Microsporum_canis
"""
Microsporum canis has been identified as a causal agent of a ringworm infection in pets, tinea capitis and tinea corporis in humans, children in particular. [...] Microsporum canis produces infections of scalp and body sites, creating highly inflammatory lesions associated with hair loss.[3] Infection by this species can often be detected clinically using Wood's lamp, which causes infected tissues to fluoresce bright green
"""
https://en.wikipedia.org/wiki/Tinea_capitis
https://en.wikipedia.org/wiki/Tinea_corporis
"""
Tinea corporis is a fungal infection of the body, similar to other forms of tinea. Specifically, it is a type of dermatophytosis (or ringworm) that appears on the arms and legs, especially on glabrous skin; however, it may occur on any superficial part of the body.
[...]
It may have a variety of appearances; most easily identifiable are the enlarging raised red rings with a central area of clearing (ringworm).[3] The same appearances of ringworm may also occur on the scalp (tinea capitis), beard area (tinea barbae) or the groin (tinea cruris, known as jock itch or dhobi itch).
[...]
Other classic features of tinea corporis include:
The disease can also be acquired by person-to-person transfer usually via direct skin contact with an infected individual.[3] Animal-to-human transmission is also common. Ringworm commonly occurs on pets (dogs, cats) and the fungus can be acquired while petting or grooming an animal. Ringworm can also be acquired from other animals such as horses, pigs, ferrets and cows. The fungus can also be spread by touching inanimate objects like personal care products, bed linen, combs, athletic gear, or hair brushes contaminated by an affected person.[3]
"""
(diagnosis)
"""
Superficial scrapes of skin examined underneath a microscope may reveal the presence of a fungus. This is done by utilizing a diagnostic method called KOH test
"""
https://en.wikipedia.org/wiki/KOH_test
"""
The KOH Test for Candida albicans, also known as a potassium hydroxide preparation or KOH prep, is a quick, inexpensive fungal test to differentiate dermatophytes and Candida albicans symptoms from other skin disorders like psoriasis and eczema.[1]
[...]
The KOH prep cannot identify the specific organism; the specimen can be submitted for fungal culture to identify the organism.
"""
"""
Microsporidian infections of humans sometimes cause a disease called microsporidiosis. At least 14 microsporidian species, spread across eight genera, have been recognized as human pathogens. These include Trachipleistophora hominis.[24]
"""
"""
Treatment
Microsporum canis infections can be easily managed by topical antifungal agents; however severe cases may necessitate systemic therapy with griseofulvin, itraconazole or terbinafine.[1][9] Treatment of human cases also requires the identification and elimination of the infectious reservoir, which typically involves the investigation and treatment of colonized animals and the elimination of infected bedding and other environmental reservoirs.[10]
"""
https://en.wikipedia.org/wiki/Microsporidiosis
Tinea microsporica
###
https://en.wikipedia.org/wiki/Encephalitozoon_intestinalis
https://en.wikipedia.org/wiki/Enterocytozoon_bieneusi
"""
Enterocytozoon bieneusi is a species of the order Chytridiopsida (in the division Microsporidia) which infects the intestinal epithelial cells. It is an obligate intracellular parasite.[1]
[...]
Study and detection methods
Light microscopy of stained clinical smears, especially of fecal samples, is used to diagnose microsporidia infections.. Transmission electron microscopy is required to differentiate between species of microsporidia, but it is time consuming and expensive. Immunofluorescence Assays using monoclonal and polyclonal antibodies are used, and PCR has recently been employed for E. bieneusi (CDC).
[...]
Enerocytozoon bieneusi is transported through environment resistant spores.
Common environmental sources of E. bieneusi include ditch and other surface waters, and several species of microsporidia can be isolated from such sources indicating that the disease may be waterborne. [...] there seem to be a close relationship between E. bieneusi strains from humans and pigs, suggesting the absence of transmission barrier between pigs and humans for this parasite (Rinder et al. 2000).
[...]
PCR analysis in Czech Republic revealed existence of E. bieneusi in 94% of the samples indicating the large presence of E. bieneusi in swine, and that they may be naturally occurring (Sak et al. 2008).
[...]
Moreover, these pigs can serve as zoonotic reservoirs for E. bieneusi, making transmission to other animals and humans possible. Since the transmission from swine to other humans and animals is not studied yet, this may cause a major impact on the health of this country
"""
______________
https://en.wikipedia.org/wiki/Microsporidia
(general family, about 10% infect humans)
(SLO): https://sl.wikipedia.org/wiki/Mikrosporija / mikrosporoza
(DE): https://de.wikipedia.org/wiki/Mikrosporie
Many can be gotten from pets, like Microspirosis
"""
Bolezen pogosto povzroča Microsporum canis in se na ljudi po navadi prenese z mačk, redkeje s psov. Redkejša povzročitelja mokrosporije sta M. gypseum (zoofilni dermatofit) in M. audouinii (antropofilni dermatofit). Vir okužbe so najpogosteje živali v okolici, obolevajo zlasti šolski otroci. Pogostejša je pri ženskem spolu ter od julija do oktobra.
"""
http://iloveanimalfriends.over-blog.com/2015/10/microsporosis-in-your-pets.html
"""
Microsporosis in the cats (less frequently in dogs) manifests in one or more areas of alopecia or without hair on the animal's body. These changes to the skin can be substantially round, oval or irregularly shaped.
[...]
There are two forms Microsporosis in humans, depending on the location:
If the infected scalp hair in these places waste in circles or oval surfaces and has a height of two to four millimeters above the skin.
In the case of contamination of other parts of the body there are changes in the skin in the form of circles with a raised edge in red, while the interior of the circle normal color (in the image). Also, there is also fine scaling in the middle rounds as possible are less crusting. Changes may be accompanied by moderate or intense itching.
"""
______________
https://en.wikipedia.org/wiki/Microsporum_canis
"""
Microsporum canis has been identified as a causal agent of a ringworm infection in pets, tinea capitis and tinea corporis in humans, children in particular. [...] Microsporum canis produces infections of scalp and body sites, creating highly inflammatory lesions associated with hair loss.[3] Infection by this species can often be detected clinically using Wood's lamp, which causes infected tissues to fluoresce bright green
"""
https://en.wikipedia.org/wiki/Tinea_capitis
https://en.wikipedia.org/wiki/Tinea_corporis
"""
Tinea corporis is a fungal infection of the body, similar to other forms of tinea. Specifically, it is a type of dermatophytosis (or ringworm) that appears on the arms and legs, especially on glabrous skin; however, it may occur on any superficial part of the body.
[...]
It may have a variety of appearances; most easily identifiable are the enlarging raised red rings with a central area of clearing (ringworm).[3] The same appearances of ringworm may also occur on the scalp (tinea capitis), beard area (tinea barbae) or the groin (tinea cruris, known as jock itch or dhobi itch).
[...]
Other classic features of tinea corporis include:
- Itching occurs on infected area.
- The edge of the rash appears elevated and is scaly to touch.
- Sometimes the skin surrounding the rash may be dry and flaky.
- Almost invariably, there will be hair loss in areas of the infection.[4]
The disease can also be acquired by person-to-person transfer usually via direct skin contact with an infected individual.[3] Animal-to-human transmission is also common. Ringworm commonly occurs on pets (dogs, cats) and the fungus can be acquired while petting or grooming an animal. Ringworm can also be acquired from other animals such as horses, pigs, ferrets and cows. The fungus can also be spread by touching inanimate objects like personal care products, bed linen, combs, athletic gear, or hair brushes contaminated by an affected person.[3]
"""
(diagnosis)
"""
Superficial scrapes of skin examined underneath a microscope may reveal the presence of a fungus. This is done by utilizing a diagnostic method called KOH test
"""
https://en.wikipedia.org/wiki/KOH_test
"""
The KOH Test for Candida albicans, also known as a potassium hydroxide preparation or KOH prep, is a quick, inexpensive fungal test to differentiate dermatophytes and Candida albicans symptoms from other skin disorders like psoriasis and eczema.[1]
[...]
The KOH prep cannot identify the specific organism; the specimen can be submitted for fungal culture to identify the organism.
"""
"""
Microsporidian infections of humans sometimes cause a disease called microsporidiosis. At least 14 microsporidian species, spread across eight genera, have been recognized as human pathogens. These include Trachipleistophora hominis.[24]
"""
"""
Treatment
Microsporum canis infections can be easily managed by topical antifungal agents; however severe cases may necessitate systemic therapy with griseofulvin, itraconazole or terbinafine.[1][9] Treatment of human cases also requires the identification and elimination of the infectious reservoir, which typically involves the investigation and treatment of colonized animals and the elimination of infected bedding and other environmental reservoirs.[10]
"""
https://en.wikipedia.org/wiki/Microsporidiosis
Tinea microsporica
###
https://en.wikipedia.org/wiki/Encephalitozoon_intestinalis
https://en.wikipedia.org/wiki/Enterocytozoon_bieneusi
"""
Enterocytozoon bieneusi is a species of the order Chytridiopsida (in the division Microsporidia) which infects the intestinal epithelial cells. It is an obligate intracellular parasite.[1]
[...]
Study and detection methods
Light microscopy of stained clinical smears, especially of fecal samples, is used to diagnose microsporidia infections.. Transmission electron microscopy is required to differentiate between species of microsporidia, but it is time consuming and expensive. Immunofluorescence Assays using monoclonal and polyclonal antibodies are used, and PCR has recently been employed for E. bieneusi (CDC).
[...]
Enerocytozoon bieneusi is transported through environment resistant spores.
Common environmental sources of E. bieneusi include ditch and other surface waters, and several species of microsporidia can be isolated from such sources indicating that the disease may be waterborne. [...] there seem to be a close relationship between E. bieneusi strains from humans and pigs, suggesting the absence of transmission barrier between pigs and humans for this parasite (Rinder et al. 2000).
[...]
PCR analysis in Czech Republic revealed existence of E. bieneusi in 94% of the samples indicating the large presence of E. bieneusi in swine, and that they may be naturally occurring (Sak et al. 2008).
[...]
Moreover, these pigs can serve as zoonotic reservoirs for E. bieneusi, making transmission to other animals and humans possible. Since the transmission from swine to other humans and animals is not studied yet, this may cause a major impact on the health of this country
"""
______________
https://en.wikipedia.org/wiki/Microsporidia
(general family, about 10% infect humans)
¶EARWIGS
ewwww
https://www.healthline.com/health/earwig-bite#causes
https://www.terminix.com/blog/bug-facts/what-are-earwigs/
ewwww
https://www.healthline.com/health/earwig-bite#causes
https://www.terminix.com/blog/bug-facts/what-are-earwigs/
¶MITES
There's many different kinds.
They're tiny, often misdiagenosed, and currently underestimated.
https://content.ces.ncsu.edu/mites-that-bug-people
https://mitetreatments.com/top-ten-mite-questions/391-2/
nice starter faq ;-)
There's many different kinds.
They're tiny, often misdiagenosed, and currently underestimated.
https://content.ces.ncsu.edu/mites-that-bug-people
https://mitetreatments.com/top-ten-mite-questions/391-2/
nice starter faq ;-)
¶ mite: Scabies
esp: "Sarna"
slo: "Garje", "Srbečica"
___________________
"""
The eight-legged mite that causes scabies in humans is microscopic. The female mite burrows just beneath your skin and makes a tunnel where it deposits eggs."
The eggs hatch, and the mite larvae work their way to the surface of your skin, where they mature and can spread to other areas of your skin or to the skin of other people. The itching of scabies results from your body's allergic reaction to the mites, their eggs and their waste.
"""
https://en.wikipedia.org/wiki/Scabies
www.pcds.org.uk/clinical-guidance/scabies
https://www.medicinenet.com/image-collection/scabies_picture/picture.htm
ID photos
https://www.medicinenet.com/scabies/article.htm
info + q&a
https://www.mayoclinic.org/diseases-conditions/scabies/symptoms-causes/syc-20377378
info, spots,
http://examnnotes.com/Scabies.html
"""
Scabies, also known as the seven-year itch, is a contagious skin infestation by the mite Sarcoptes scabiei.[3][1] The most common symptoms are severe itchiness and a pimple-like rash.[2] Occasionally, tiny burrows may be seen in the skin.[2] In a first-ever infection a person will usually develop symptoms in between two and six weeks.[2] During a second infection symptoms may begin in as little as 24 hours.[2] These symptoms can be present across most of the body or just certain areas such as the wrists, between fingers, or along the waistline.
"""

__________
diagnosis:
"The burrow tracks are often linear, to the point that a neat "line" of four or more closely placed and equally developed mosquito-like "bites" is almost diagnostic of the disease"
A) To detect the burrow, the suspected area is rubbed with ink from a fountain pen or a topical tetracycline solution, which glows under a special light. The skin is then wiped with an alcohol pad. If the person is infected with scabies, the characteristic zigzag or S pattern of the burrow will appear across the skin; however, interpreting this test may be difficult, as the burrows are scarce and may be obscured by scratch marks.[11]
_________________
!!!:
what fountain pen?
how can this be improvised?
info:
* https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222761/ :
!!
→ "Detection of scabies: A systematic review of diagnostic methods"
* [...]
B) A definitive diagnosis is made by finding either the scabies mites or their eggs and fecal pellets.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1865595/
"""
In humans, the symptoms of scabies infestations can mimic other dermatological skin diseases, and traditional tests to diagnose scabies are less than 50% accurate. To aid early identification of disease and thus treatment, a simple, cheap, sensitive, and specific test for routine diagnosis of active scabies is essential. Recent
"""
often atypical:
forming papules and nodules
https://www.dovepress.com/scabies-masquerading-as-bullous-pemphigoid-scabies-surrepticius-peer-reviewed-fulltext-article-CCID
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7186094/
"Classic and Non-classic (Surrepticius) Scabies: Diagnostic and Treatment Considerations"
___________
spread:
"""About 1–10% of the global population is estimated to be infected with scabies, but in certain populations, the infection rate may be as high as 50–80%."""
_________
Number + "Crusted scabies" ("norwegian scabies") variant
"""
Normally, someone with scabies has about 10 to 15 mites.
In contrast, someone with crusted scabies may be infested with millions of mites.
"""
_________
Treatment
"""The mite does not live for more than 3 days away from human skin"""
atypical:
* underwater?
* in salt? https://patient.info/forums/discuss/i-was-very-happy-to-find-that-common-table-salt-in-a-war--3361
* essential oils: [...]
* [...]
esp: "Sarna"
slo: "Garje", "Srbečica"
___________________
"""
The eight-legged mite that causes scabies in humans is microscopic. The female mite burrows just beneath your skin and makes a tunnel where it deposits eggs."
The eggs hatch, and the mite larvae work their way to the surface of your skin, where they mature and can spread to other areas of your skin or to the skin of other people. The itching of scabies results from your body's allergic reaction to the mites, their eggs and their waste.
"""
https://en.wikipedia.org/wiki/Scabies
www.pcds.org.uk/clinical-guidance/scabies
https://www.medicinenet.com/image-collection/scabies_picture/picture.htm
ID photos
https://www.medicinenet.com/scabies/article.htm
info + q&a
https://www.mayoclinic.org/diseases-conditions/scabies/symptoms-causes/syc-20377378
info, spots,
http://examnnotes.com/Scabies.html
"""
Scabies, also known as the seven-year itch, is a contagious skin infestation by the mite Sarcoptes scabiei.[3][1] The most common symptoms are severe itchiness and a pimple-like rash.[2] Occasionally, tiny burrows may be seen in the skin.[2] In a first-ever infection a person will usually develop symptoms in between two and six weeks.[2] During a second infection symptoms may begin in as little as 24 hours.[2] These symptoms can be present across most of the body or just certain areas such as the wrists, between fingers, or along the waistline.
"""

__________
diagnosis:
"The burrow tracks are often linear, to the point that a neat "line" of four or more closely placed and equally developed mosquito-like "bites" is almost diagnostic of the disease"
A) To detect the burrow, the suspected area is rubbed with ink from a fountain pen or a topical tetracycline solution, which glows under a special light. The skin is then wiped with an alcohol pad. If the person is infected with scabies, the characteristic zigzag or S pattern of the burrow will appear across the skin; however, interpreting this test may be difficult, as the burrows are scarce and may be obscured by scratch marks.[11]
_________________
!!!:
what fountain pen?
how can this be improvised?
info:
* https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222761/ :
!!
→ "Detection of scabies: A systematic review of diagnostic methods"
* [...]
B) A definitive diagnosis is made by finding either the scabies mites or their eggs and fecal pellets.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1865595/
"""
In humans, the symptoms of scabies infestations can mimic other dermatological skin diseases, and traditional tests to diagnose scabies are less than 50% accurate. To aid early identification of disease and thus treatment, a simple, cheap, sensitive, and specific test for routine diagnosis of active scabies is essential. Recent
"""
often atypical:
forming papules and nodules
https://www.dovepress.com/scabies-masquerading-as-bullous-pemphigoid-scabies-surrepticius-peer-reviewed-fulltext-article-CCID
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7186094/
"Classic and Non-classic (Surrepticius) Scabies: Diagnostic and Treatment Considerations"
___________
spread:
"""About 1–10% of the global population is estimated to be infected with scabies, but in certain populations, the infection rate may be as high as 50–80%."""
_________
Number + "Crusted scabies" ("norwegian scabies") variant
"""
Normally, someone with scabies has about 10 to 15 mites.
In contrast, someone with crusted scabies may be infested with millions of mites.
"""
_________
Treatment
"""The mite does not live for more than 3 days away from human skin"""
atypical:
* underwater?
* in salt? https://patient.info/forums/discuss/i-was-very-happy-to-find-that-common-table-salt-in-a-war--3361
* essential oils: [...]
* [...]
¶ mite: Chiggers
horrible little red shits.
they spread typhus as well.
______________
https://en.wikipedia.org/wiki/Trombiculidae
"""The Trombiculidae (/trɒmbɪˈkjuːlɪdiː/; also called berry bugs, harvest mites, red bugs, scrub-itch mites, and aoutas) are a family of mites.[3] The best known of the Trombiculidae are chiggers. The two widely recognized definitions of "chigger" are the scientific (or taxonomic) and the common, the latter of which can be found in English and medical[4] dictionaries"""
"""
They do not actually "bite", but instead form a hole in the skin called a stylostome and chew up tiny parts of the inner skin, thus causing severe irritation and swelling. The severe itching is accompanied by red, pimple-like bumps (papules) or hives and skin rash or lesions on a sun-exposed area. For humans, itching usually occurs after the larvae detach from the skin.
"""
horrible little red shits.
they spread typhus as well.
______________
https://en.wikipedia.org/wiki/Trombiculidae
"""The Trombiculidae (/trɒmbɪˈkjuːlɪdiː/; also called berry bugs, harvest mites, red bugs, scrub-itch mites, and aoutas) are a family of mites.[3] The best known of the Trombiculidae are chiggers. The two widely recognized definitions of "chigger" are the scientific (or taxonomic) and the common, the latter of which can be found in English and medical[4] dictionaries"""
"""
They do not actually "bite", but instead form a hole in the skin called a stylostome and chew up tiny parts of the inner skin, thus causing severe irritation and swelling. The severe itching is accompanied by red, pimple-like bumps (papules) or hives and skin rash or lesions on a sun-exposed area. For humans, itching usually occurs after the larvae detach from the skin.
"""
¶ Red mites / Avian mites → Dermanyssus gallinae
aka:
"""Red mite, bird mite, poultry mite, red poultry mite, roost mite, chicken mite, pigeon mite"""
ESP: "acaros rojos"
They are tiny!
https://en.wikipedia.org/wiki/Dermanyssus_gallinae
"""
Dermanyssus gallinae (also known as the red mite) is a haematophagous ectoparasite of poultry. It has been implicated as a vector of several major pathogenic diseases.[1] Despite its common names, it has a wide range of hosts including several species of wild birds and mammals, including humans.[2][3] In both size and appearance, it resembles the northern fowl mite, Ornithonyssus sylviarum.[4]
"""
* associated with hens, but can produce human infestations
* """In humans, D. gallinae infestations are known as gamasoidosis or dermanyssosis.[21] The mites are capable of digesting[22] and reproducing entirely on human blood, so infestations can be persistent.[3] Due to the nocturnal feeding habits of D. gallinae, infested people may experience itching and notice bites when they wake up in the morning.[23] The severity of symptoms vary, with dermatitis,[24] pruritus and papular urticaria being common.[21]"""
* """can survive for up to 10 months in an empty hen house, temperatures greater than 45 °C/113 °F and less than -20 °C/-4 °F, have been found to be lethal.[11]"""
* [...]
_____________
lol #antipest literature ...
"""Jane Ishka recited her experience with a human D. gallinae infestation in her book The Year of the Mite.[29]"""
_______________
??? This spanish article connects Red mites to Alpha-gal allergy.
Usually it's associated with tick bites !
https://www.infoalergico.com/index.php?option=com_content&view=article&id=2513:las-picaduras-de-acaro-rojo-pueden-producir-una-reaccion-alergica-a-la-carne-roja&catid=93:investigacion
___________________________________________________
https://en.wikipedia.org/wiki/Gamasoidosis
"""
Gamasoidosis or dermanyssosis is a frequently unrecognized ectoparasitosis[2] and source of growing concern in human medicine,[3] occurring after contact with avian mites which infest canaries,[4] sparrows, starlings, pigeons[5] and poultry[6] and caused by two genera of mites, Ornithonyssus and Dermanyssus.[7] Avian mite species implicated include the red mite (Dermanyssus gallinae),[8] tropical fowl mite (Ornithonyssus bursa)[9] and northern fowl mite (Ornithonyssus sylviarum)[8]. Mite dermatitis is also associated with rodents infested with the tropical rat mite (Ornithonyssus bacoti),[10][11] spiny rat mite (Laelaps echidnina)[12] and house-mouse mite (Liponyssoides sanguineus), where the condition is known as rodent mite dermatitis.[13] Urban gamasoidosis is associated with window-sills, ventilation and air-conditioning intakes, rooves and eaves, which serve as shelters for nesting birds. Humans bitten by these mites experience a non-specific dermatitis with intense itching.[14][15]
"""
----------------
"""
Bites are normally located in groups around the neck and body areas covered by clothes (waist, trunk, upper extremities and abdomen),[3][10][17] but can also be found on the legs,[14] finger webs, axillae, the groin, and buttocks.[17] If feeding occurs while a patient is sleeping, bedclothes and pillows may show red spots caused by droppings or crushed mites.[3]
D. gallinae is capable of infesting the ear canal, with symptoms including itching, internal inflammation and discharge.[18] It can also infest the scalp, with severe itching — particularly at night as the primary symptom[19] — as well as "the nares, orbits and eyelids, and genitourinary and rectal orifices.“[20]
"""
FINDING !!!:
"""Diagnosis can be challenging as the small size of avian mites make them "barely visible to the unaided eye".[22] Identification of the species is best carried out by a medical entomologist using a microscope,[8] positive identification of species is critical for recommendation of suitable treatment. Samples can be obtained using corrugated cardboard traps, left in infested areas.[23]"""
"""
Due to it being an uncommon diagnosis, physicians are generally not aware of the condition,[3] meaning gamasoidosis may be misdiagnosed as scabies or pediculosis[25] or bites mistakenly identified as coming from bed bugs.[26] Many cases of gamasoidosis go unreported, suggesting that the actual incidence is higher than generally believed
"""
"""
. gallinae may be commonly found in the bedroom or where the patient sleeps, as they prefer to stay close to their host for optimal feeding.[30] They are attracted to warm hiding places that simulate the body temperature of birds (e.g. pigeons 42 °C), "such as the electrical devices running in stand-by mode (e.g. laptop computers, television, radio clocks etc.)" which generate heat. As a result, "it is strongly recommended to check these electrical appliances for the mite detection".[14] D. gallinae generally visit their host for up to 1–2 hours, leave after completing their blood meal[14] and typically feed every 2–4 days.[24] They are able to move extremely quickly[16] and can take less than 1 second to bite, enough time to inject their saliva and to induce rash and itching.[14] They locate potential hosts through temperature changes,[14] vibration and CO².[31][32]
"""
FUCK ME
TREATMENT
"""
Patients are advised to:[3][14]
"""
Certain essential oils are known to have an acaricide effect on avian mites.[45]
Cardboard traps impregnated with neem extracts or other acaricides[46] can be used to reduce avian mite populations.[47]
"""
MORE PATHOGENS !
bloody fuck, what is all this shit
"""
D. gallinae poses a significant threat to public health as the mite may be vector/reservoir of several zoonotic pathogens,[24] such as:
* Chlamydia psittaci,
* Erysipelothrix rhusiopathiae,
* Salmonella spp.,
* Lyme disease,[24]
* Mycobacterium spp.,
* Coxiella burnetii,
* Bartonella spp.,[26]
* Borrelia burgdorferi,[48]
* Venezuelan equine encephalitis virus,
* Eastern equine encephalitis virus, and
* Fowlpox virus.[49]
"""
aka:
"""Red mite, bird mite, poultry mite, red poultry mite, roost mite, chicken mite, pigeon mite"""
ESP: "acaros rojos"
They are tiny!
https://en.wikipedia.org/wiki/Dermanyssus_gallinae
"""
Dermanyssus gallinae (also known as the red mite) is a haematophagous ectoparasite of poultry. It has been implicated as a vector of several major pathogenic diseases.[1] Despite its common names, it has a wide range of hosts including several species of wild birds and mammals, including humans.[2][3] In both size and appearance, it resembles the northern fowl mite, Ornithonyssus sylviarum.[4]
"""
* associated with hens, but can produce human infestations
* """In humans, D. gallinae infestations are known as gamasoidosis or dermanyssosis.[21] The mites are capable of digesting[22] and reproducing entirely on human blood, so infestations can be persistent.[3] Due to the nocturnal feeding habits of D. gallinae, infested people may experience itching and notice bites when they wake up in the morning.[23] The severity of symptoms vary, with dermatitis,[24] pruritus and papular urticaria being common.[21]"""
* """can survive for up to 10 months in an empty hen house, temperatures greater than 45 °C/113 °F and less than -20 °C/-4 °F, have been found to be lethal.[11]"""
* [...]
_____________
lol #antipest literature ...
"""Jane Ishka recited her experience with a human D. gallinae infestation in her book The Year of the Mite.[29]"""
_______________
??? This spanish article connects Red mites to Alpha-gal allergy.
Usually it's associated with tick bites !
https://www.infoalergico.com/index.php?option=com_content&view=article&id=2513:las-picaduras-de-acaro-rojo-pueden-producir-una-reaccion-alergica-a-la-carne-roja&catid=93:investigacion
___________________________________________________
https://en.wikipedia.org/wiki/Gamasoidosis
"""
Gamasoidosis or dermanyssosis is a frequently unrecognized ectoparasitosis[2] and source of growing concern in human medicine,[3] occurring after contact with avian mites which infest canaries,[4] sparrows, starlings, pigeons[5] and poultry[6] and caused by two genera of mites, Ornithonyssus and Dermanyssus.[7] Avian mite species implicated include the red mite (Dermanyssus gallinae),[8] tropical fowl mite (Ornithonyssus bursa)[9] and northern fowl mite (Ornithonyssus sylviarum)[8]. Mite dermatitis is also associated with rodents infested with the tropical rat mite (Ornithonyssus bacoti),[10][11] spiny rat mite (Laelaps echidnina)[12] and house-mouse mite (Liponyssoides sanguineus), where the condition is known as rodent mite dermatitis.[13] Urban gamasoidosis is associated with window-sills, ventilation and air-conditioning intakes, rooves and eaves, which serve as shelters for nesting birds. Humans bitten by these mites experience a non-specific dermatitis with intense itching.[14][15]
"""
----------------
"""
Bites are normally located in groups around the neck and body areas covered by clothes (waist, trunk, upper extremities and abdomen),[3][10][17] but can also be found on the legs,[14] finger webs, axillae, the groin, and buttocks.[17] If feeding occurs while a patient is sleeping, bedclothes and pillows may show red spots caused by droppings or crushed mites.[3]
D. gallinae is capable of infesting the ear canal, with symptoms including itching, internal inflammation and discharge.[18] It can also infest the scalp, with severe itching — particularly at night as the primary symptom[19] — as well as "the nares, orbits and eyelids, and genitourinary and rectal orifices.“[20]
"""
FINDING !!!:
"""Diagnosis can be challenging as the small size of avian mites make them "barely visible to the unaided eye".[22] Identification of the species is best carried out by a medical entomologist using a microscope,[8] positive identification of species is critical for recommendation of suitable treatment. Samples can be obtained using corrugated cardboard traps, left in infested areas.[23]"""
"""
Due to it being an uncommon diagnosis, physicians are generally not aware of the condition,[3] meaning gamasoidosis may be misdiagnosed as scabies or pediculosis[25] or bites mistakenly identified as coming from bed bugs.[26] Many cases of gamasoidosis go unreported, suggesting that the actual incidence is higher than generally believed
"""
"""
. gallinae may be commonly found in the bedroom or where the patient sleeps, as they prefer to stay close to their host for optimal feeding.[30] They are attracted to warm hiding places that simulate the body temperature of birds (e.g. pigeons 42 °C), "such as the electrical devices running in stand-by mode (e.g. laptop computers, television, radio clocks etc.)" which generate heat. As a result, "it is strongly recommended to check these electrical appliances for the mite detection".[14] D. gallinae generally visit their host for up to 1–2 hours, leave after completing their blood meal[14] and typically feed every 2–4 days.[24] They are able to move extremely quickly[16] and can take less than 1 second to bite, enough time to inject their saliva and to induce rash and itching.[14] They locate potential hosts through temperature changes,[14] vibration and CO².[31][32]
"""
FUCK ME
TREATMENT
"""
Patients are advised to:[3][14]
- Shower frequently to remove mites from their skin and hair.
- Washing clothes and bedding at temperatures, at or above 60 °C.
- Remove the source of the mites, such as infested animal shelters, cages and nests.
- Perform regular intensive vacuum cleaning and steam cleaning — the vacuum bag should be placed in a sealed bag and thrown away outside in a contained bin.
- Disinfect infested household items and areas with effective acaricides such as pyrethroids.
- Washing of textiles or steam cleaning (cushions, carpets, curtains) at or above 60 °C, and drying them using an automated laundry drier.
- Dust infested areas with amorphous silica gels[41] such as CimeXa.[42]
- Heat treat their residence — raising the temperature of their living space above 55 °C for a sustained period.
- Reduce the relative humidity of their home below 55%.[36]
"""
Certain essential oils are known to have an acaricide effect on avian mites.[45]
Cardboard traps impregnated with neem extracts or other acaricides[46] can be used to reduce avian mite populations.[47]
"""
MORE PATHOGENS !
bloody fuck, what is all this shit
"""
D. gallinae poses a significant threat to public health as the mite may be vector/reservoir of several zoonotic pathogens,[24] such as:
* Chlamydia psittaci,
* Erysipelothrix rhusiopathiae,
* Salmonella spp.,
* Lyme disease,[24]
* Mycobacterium spp.,
* Coxiella burnetii,
* Bartonella spp.,[26]
* Borrelia burgdorferi,[48]
* Venezuelan equine encephalitis virus,
* Eastern equine encephalitis virus, and
* Fowlpox virus.[49]
"""
¶ mites → Sarcoptic mange (hair/skin disease)
mange
https://en.wikipedia.org/wiki/Mange
"""
Mange /ˈmeɪndʒ/ is a type of skin disease caused by parasitic mites.[1] Because mites also infect plants, birds, and reptiles, the term "mange", suggesting poor condition of the hairy coat due to the infection, is sometimes reserved only for pathological mite-infestation of nonhuman mammals.
[...]
Thus, mange includes mite-associated skin disease in domestic animals (cats and dogs), in livestock (such as sheep scab), and in wild animals (for example, coyotes, cougars, and bears).[2][3] Since mites belong to the arachnid subclass Acari (also called Acarina), another term for mite infestation is acariasis.
Parasitic mites that cause mange in mammals embed themselves in either skin or hair follicles in the animal, depending upon their genus. Sarcoptes spp. burrow into skin, while Demodex spp. live in follicles.
In humans, these two types of mite infections, which would otherwise be known as "mange" in furry mammals, are instead known respectively as scabies and demodicosis.
"""
sarcoptic mange (dogs)
You will get it from the dog. It will itch but die and not spread.
https://vcahospitals.com/know-your-pet/mange-sarcoptic-in-dogs
"""
What does it do to the dog?
The presence of the sarcoptic mite causes intense itching. The dog will chew and scratch its skin constantly. This leads to the loss of large amounts of hair, especially on the legs and belly. Eventually, the skin will become thickened and will darken.
Is it contagious?
Yes. Sarcoptic mange is highly contagious to other dogs and humans.
Although sarcoptic mites are not able to complete their life cycle on humans, they will cause severe itching until they die.
"""
notoedric mange (cats)
https://en.wikipedia.org/wiki/Notoedric_mange
in humans:
"""
Infestation of N. cati causes several symptoms such as severe itchiness, alopecia, scales and characteristic dry, crusted, pruritic lesions that first appear in the region of the ears and rapidly spreads over the face, eyelids, neck and continues to infest the whole body.[5][6] Clinical symptoms appear within the incubation period, which is most commonly 10 days to 8 weeks after transmission has happened from contact with an infested animal.[7] Skin will become thickened and colour of crusting will change yellowish or grey as the parasitic disease progresses.[6][8][7] Self-trauma because of severe itching can cause excoriations to develop severe dermatitis, secondary bacterial infections. Far progressed Notoedric mange often leads to apathy, anorexia and even death.[9] In humans, infestation of N.cati can result in transient pruritic lesions.[10]
"""
mange
https://en.wikipedia.org/wiki/Mange
"""
Mange /ˈmeɪndʒ/ is a type of skin disease caused by parasitic mites.[1] Because mites also infect plants, birds, and reptiles, the term "mange", suggesting poor condition of the hairy coat due to the infection, is sometimes reserved only for pathological mite-infestation of nonhuman mammals.
[...]
Thus, mange includes mite-associated skin disease in domestic animals (cats and dogs), in livestock (such as sheep scab), and in wild animals (for example, coyotes, cougars, and bears).[2][3] Since mites belong to the arachnid subclass Acari (also called Acarina), another term for mite infestation is acariasis.
Parasitic mites that cause mange in mammals embed themselves in either skin or hair follicles in the animal, depending upon their genus. Sarcoptes spp. burrow into skin, while Demodex spp. live in follicles.
In humans, these two types of mite infections, which would otherwise be known as "mange" in furry mammals, are instead known respectively as scabies and demodicosis.
"""
sarcoptic mange (dogs)
You will get it from the dog. It will itch but die and not spread.
https://vcahospitals.com/know-your-pet/mange-sarcoptic-in-dogs
"""
What does it do to the dog?
The presence of the sarcoptic mite causes intense itching. The dog will chew and scratch its skin constantly. This leads to the loss of large amounts of hair, especially on the legs and belly. Eventually, the skin will become thickened and will darken.
Is it contagious?
Yes. Sarcoptic mange is highly contagious to other dogs and humans.
Although sarcoptic mites are not able to complete their life cycle on humans, they will cause severe itching until they die.
"""
notoedric mange (cats)
https://en.wikipedia.org/wiki/Notoedric_mange
in humans:
"""
Infestation of N. cati causes several symptoms such as severe itchiness, alopecia, scales and characteristic dry, crusted, pruritic lesions that first appear in the region of the ears and rapidly spreads over the face, eyelids, neck and continues to infest the whole body.[5][6] Clinical symptoms appear within the incubation period, which is most commonly 10 days to 8 weeks after transmission has happened from contact with an infested animal.[7] Skin will become thickened and colour of crusting will change yellowish or grey as the parasitic disease progresses.[6][8][7] Self-trauma because of severe itching can cause excoriations to develop severe dermatitis, secondary bacterial infections. Far progressed Notoedric mange often leads to apathy, anorexia and even death.[9] In humans, infestation of N.cati can result in transient pruritic lesions.[10]
"""
¶ mite: Demodex ("eyelash mites")
https://en.wikipedia.org/wiki/Demodex
https://www.healthline.com/health/demodex-folliculorum
Lives in most adult people on eyebrows & eyelashes
"""
Demodex is a genus of tiny mites that live in or near hair follicles of mammals. Around 65 species of Demodex are known.[2] Two species live on humans: Demodex folliculorum and Demodex brevis, both frequently referred to as eyelash mites
"""
"The adult mites are only 0.3–0.4 mm (0.012–0.016 in) long, with D. brevis slightly shorter than D. folliculorum"
"Older people are much more likely to carry the mites; about a third of children and young adults, half of adults, and two-thirds of elderly people carry them"
May cause acne and rosacea!
https://en.wikipedia.org/wiki/Rosacea#Demodex_mites
TREATMENT:
* https://www.longdom.org/open-access/impact-of-salvia-and-peppermint-oil-on-the-in-vitro-survival-of-demodex-mites-2155-9597-1000227.pdf :
salvia & peppermint
* [...]
_______________
connected to conjunctivitis?
"""
The Demodicidae family includes strictly specialized parasitic mitesliving in the skin, hair follicles or outer epidermal layers. Demodexmites show strong host-species specificity. Up to now, two human-specific Demodex species have been described: Demodexfolliculorumand Demodex brevis. These mites may cause ocular demodicosis withsymptoms such as burning and itching of eyelids. Demodex plays animportant role in Demodex blepharitis, meibomian gland dysfunction,conjunctival inflammation or corneal lesions [1
"""
https://en.wikipedia.org/wiki/Demodex
https://www.healthline.com/health/demodex-folliculorum
Lives in most adult people on eyebrows & eyelashes
"""
Demodex is a genus of tiny mites that live in or near hair follicles of mammals. Around 65 species of Demodex are known.[2] Two species live on humans: Demodex folliculorum and Demodex brevis, both frequently referred to as eyelash mites
"""
"The adult mites are only 0.3–0.4 mm (0.012–0.016 in) long, with D. brevis slightly shorter than D. folliculorum"
"Older people are much more likely to carry the mites; about a third of children and young adults, half of adults, and two-thirds of elderly people carry them"
May cause acne and rosacea!
https://en.wikipedia.org/wiki/Rosacea#Demodex_mites
TREATMENT:
* https://www.longdom.org/open-access/impact-of-salvia-and-peppermint-oil-on-the-in-vitro-survival-of-demodex-mites-2155-9597-1000227.pdf :
salvia & peppermint
* [...]
_______________
connected to conjunctivitis?
"""
The Demodicidae family includes strictly specialized parasitic mitesliving in the skin, hair follicles or outer epidermal layers. Demodexmites show strong host-species specificity. Up to now, two human-specific Demodex species have been described: Demodexfolliculorumand Demodex brevis. These mites may cause ocular demodicosis withsymptoms such as burning and itching of eyelids. Demodex plays animportant role in Demodex blepharitis, meibomian gland dysfunction,conjunctival inflammation or corneal lesions [1
"""
¶ mites → Acariasis
https://en.wikipedia.org/wiki/Acariasis
"""
Diagnosis
Medical doctors and dermatologists can still misdiagnose this rash as many are unfamiliar with parasitism, not trained in it, or if they do consider it, cannot see the mites.
Different methods for detection are recognized for different acariasis infections. Human acariasis with mites can occur in the gastrointestinal tract, lungs, urinary tracts and other organs which not have been well-studied. For intestinal acariasis with symptoms such as abdominal pain, diarrhea, and phohemefecia (is this hemafecia?), human acariasis is diagnosed by detection of mites in stools.[6] For pulmonary acariasis, the presence of mites in sputum is determined by identifying the presence and number of mites in the sputum of patients with respiratory symptoms. Both physical and chemical methods for liquefaction of sputum have been developed.[7]
"""
How to develop and popularise pervasive and general tests?
https://en.wikipedia.org/wiki/Acariasis
"""
Diagnosis
Medical doctors and dermatologists can still misdiagnose this rash as many are unfamiliar with parasitism, not trained in it, or if they do consider it, cannot see the mites.
Different methods for detection are recognized for different acariasis infections. Human acariasis with mites can occur in the gastrointestinal tract, lungs, urinary tracts and other organs which not have been well-studied. For intestinal acariasis with symptoms such as abdominal pain, diarrhea, and phohemefecia (is this hemafecia?), human acariasis is diagnosed by detection of mites in stools.[6] For pulmonary acariasis, the presence of mites in sputum is determined by identifying the presence and number of mites in the sputum of patients with respiratory symptoms. Both physical and chemical methods for liquefaction of sputum have been developed.[7]
"""
How to develop and popularise pervasive and general tests?
¶ Rodent mites
https://en.wikipedia.org/wiki/Rodent_mite_dermatitis
"""
Rodent mite dermatitis (also known as rat mite dermatitis) is an often unrecognized ectoparasitosis occurring after human contact with haematophagous mesostigmatid mites that infest rodents, such has house mice,[1] rats[2] and hamsters.[3] The condition is associated with the tropical rat mite (Ornithonyssus bacoti), spiny rat mite (Laelaps echidnina) and house mouse mite (Liponyssoides sanguineus)[4] which opportunistically feed on humans. Rodent mites are capable of surviving for long periods without feeding and travelling long distances when seeking hosts.[4] Cases have been reported in homes, libraries,[5] hospitals[6] and care homes.[7] A similar condition, known as gamasoidosis, is caused by avian mites.[8]
"""
OUTBREAKS:
"""Outbreaks tend to occur in older, less maintained buildings. The mite, however, can travel several hundred feet on its own if necessary to find a host and can survive for extended periods of time without a host. This, along with the nonspecific dermatitis it causes, can prevent accurate and fast diagnosis of rat mite dermatitis. The scarcity of reports, due in part to misdiagnosis and also the mildness of its symptoms, makes the disease seem less common than it is"""
DIAGNOSIS:
"""Diagnosis requires species identification of the parasite, which will be likely to be found in the environment of its host rather than on the hosts’ skin.[10] Rodent mites are very small, for O. bacoti "female mites reach a size between 0.75 and 1.40 mm, males are a little smaller".[7]"""
TREATMENT:
"""The patient's environment should then be treated,[10] using both non-residual and residual insecticides, mites crawling in the open can be removed by vacuuming or with a cloth moistened with alcohol.[12]"""
https://onlinelibrary.wiley.com/doi/pdf/10.1111/ddg.13565
"""
Since early recorded history, people who live in urban areas have shared their environment with pets and synanthropic animals, mainly birds and rodents. These animals harbor zoonotic parasites, including mites of the suborder Mesos-tigmata [ 1 ] . Among them, the avian mites Dermanyssus (D.) gallinae, Ornithonyssus (O.) sylviarum, O. bursaand the tropical rat-mite, O. bacoti are the most dermato-logically relevant species. They are non-burrowing, blood-sucking ectoparasites of similar shape and size (about 1 mm in length) [ 1 ] . With the exception of O. sylviarum, which usually lives permanently on its host, they are temporary and nocturnal visitors of their victims, hiding in daytime in their close proximity. The resting/breeding sites of birds/rodents, mainly pigeons and feral rats/mice and occasio-nally pets, act as mite reservoirs [ 2, 3 ] ; in the absence of their natural host, hungry mites may migrate into nearby human buildings and bite their inhabitants.
[...]
The parasites were identified as D. gallinae (20/26; peninsular regions), O. bacoti (4/26; Sicily/peninsular regions), O. bursa and O. sylviarum (both 1/26; Sicily) based on morphological key characters [ 1, 4 ] (Figure 3 ).
"""
https://en.wikipedia.org/wiki/Rodent_mite_dermatitis
"""
Rodent mite dermatitis (also known as rat mite dermatitis) is an often unrecognized ectoparasitosis occurring after human contact with haematophagous mesostigmatid mites that infest rodents, such has house mice,[1] rats[2] and hamsters.[3] The condition is associated with the tropical rat mite (Ornithonyssus bacoti), spiny rat mite (Laelaps echidnina) and house mouse mite (Liponyssoides sanguineus)[4] which opportunistically feed on humans. Rodent mites are capable of surviving for long periods without feeding and travelling long distances when seeking hosts.[4] Cases have been reported in homes, libraries,[5] hospitals[6] and care homes.[7] A similar condition, known as gamasoidosis, is caused by avian mites.[8]
"""
OUTBREAKS:
"""Outbreaks tend to occur in older, less maintained buildings. The mite, however, can travel several hundred feet on its own if necessary to find a host and can survive for extended periods of time without a host. This, along with the nonspecific dermatitis it causes, can prevent accurate and fast diagnosis of rat mite dermatitis. The scarcity of reports, due in part to misdiagnosis and also the mildness of its symptoms, makes the disease seem less common than it is"""
DIAGNOSIS:
"""Diagnosis requires species identification of the parasite, which will be likely to be found in the environment of its host rather than on the hosts’ skin.[10] Rodent mites are very small, for O. bacoti "female mites reach a size between 0.75 and 1.40 mm, males are a little smaller".[7]"""
TREATMENT:
"""The patient's environment should then be treated,[10] using both non-residual and residual insecticides, mites crawling in the open can be removed by vacuuming or with a cloth moistened with alcohol.[12]"""
https://onlinelibrary.wiley.com/doi/pdf/10.1111/ddg.13565
"""
Since early recorded history, people who live in urban areas have shared their environment with pets and synanthropic animals, mainly birds and rodents. These animals harbor zoonotic parasites, including mites of the suborder Mesos-tigmata [ 1 ] . Among them, the avian mites Dermanyssus (D.) gallinae, Ornithonyssus (O.) sylviarum, O. bursaand the tropical rat-mite, O. bacoti are the most dermato-logically relevant species. They are non-burrowing, blood-sucking ectoparasites of similar shape and size (about 1 mm in length) [ 1 ] . With the exception of O. sylviarum, which usually lives permanently on its host, they are temporary and nocturnal visitors of their victims, hiding in daytime in their close proximity. The resting/breeding sites of birds/rodents, mainly pigeons and feral rats/mice and occasio-nally pets, act as mite reservoirs [ 2, 3 ] ; in the absence of their natural host, hungry mites may migrate into nearby human buildings and bite their inhabitants.
[...]
The parasites were identified as D. gallinae (20/26; peninsular regions), O. bacoti (4/26; Sicily/peninsular regions), O. bursa and O. sylviarum (both 1/26; Sicily) based on morphological key characters [ 1, 4 ] (Figure 3 ).
"""
¶ (more mites)
https://en.wikipedia.org/wiki/Grocer%27s_itch
"""
Grocer's itch is a cutaneous condition characterized by a pruritic dermatitis that occurs from coming into contact with mites such as Carpoglyphus passularum (a fruit mite) or Glyciphagus domesticus (a common house mite). Contact usually occurs when handling food with mites in it, such as figs, dates, prunes, grain, cheese, or other dried foods
"""
https://en.wikipedia.org/wiki/Grain_itch
"""
Grain itch is a cutaneous condition caused by several types of mites, and characterized by intense pruritus.[1]:454
"""
https://en.wikipedia.org/wiki/Grocer%27s_itch
"""
Grocer's itch is a cutaneous condition characterized by a pruritic dermatitis that occurs from coming into contact with mites such as Carpoglyphus passularum (a fruit mite) or Glyciphagus domesticus (a common house mite). Contact usually occurs when handling food with mites in it, such as figs, dates, prunes, grain, cheese, or other dried foods
"""
https://en.wikipedia.org/wiki/Grain_itch
"""
Grain itch is a cutaneous condition caused by several types of mites, and characterized by intense pruritus.[1]:454
"""
¶Wasps
DIY trap: attract + drown
water + detergent + chicken meat
https://www.youtube.com/watch?v=7FhifTGKtUQ
#TODO @IHI !!!
DIY trap: syrup (lemonade etc) + drowning
### >L something turns around and then they cannot escape anymore
DIY trap: attract + drown
water + detergent + chicken meat
https://www.youtube.com/watch?v=7FhifTGKtUQ
¶Mice & Rats
Attacking cars / vans
* https://www.facebook.com/richrebuilds/videos/308693244156620/ :
rats destroy a Tesla
lol "they brought stuff from outside the car inside"
* cool trick for live-in vans:
leave plastic bags around, especially at suspected & crossing zones. this will alert you.
Spread Diseases
"""Diseases such as the Hantavirus, Listeria, Rat-Bite Fever and Salmonellosis among many others are brought by rats"""
Types
It's important to identify the type.
You can do this easy by different shit size/shapes
DIY poisons
* plaster of paris:
###
* with soda
https://lakenormanpest.com/baking-soda-rat-killer/
Mix equal parts sugar, oatmeal + soda bicarbona.
A rat needs to eat about 2g of soda in weight.
"""
It turns out that baking soda catalyzes some form of reaction inside the rat’s stomach. Baking soda combines with the stomach acids to produce carbon dioxide gas which rats are unable to tolerate
"""
Trapping
* DIY trap: with water + cereal:
Put a bunch of cereal into a deep enough water bowl (like an 8L water bottle)
put a straw for the mouse to walk on there
it will fall inside and drown trying to jump out
RIP mouse
* DIY trap: with oil:
https://www.youtube.com/watch?v=BxxFNkNf6q8
#TODO @krnica [!]
----------
#routine
Attacking cars / vans
* https://www.facebook.com/richrebuilds/videos/308693244156620/ :
rats destroy a Tesla
lol "they brought stuff from outside the car inside"
* cool trick for live-in vans:
leave plastic bags around, especially at suspected & crossing zones. this will alert you.
Spread Diseases
"""Diseases such as the Hantavirus, Listeria, Rat-Bite Fever and Salmonellosis among many others are brought by rats"""
Types
It's important to identify the type.
You can do this easy by different shit size/shapes
DIY poisons
* plaster of paris:
###
* with soda
https://lakenormanpest.com/baking-soda-rat-killer/
Mix equal parts sugar, oatmeal + soda bicarbona.
A rat needs to eat about 2g of soda in weight.
"""
It turns out that baking soda catalyzes some form of reaction inside the rat’s stomach. Baking soda combines with the stomach acids to produce carbon dioxide gas which rats are unable to tolerate
"""
Trapping
* DIY trap: with water + cereal:
Put a bunch of cereal into a deep enough water bowl (like an 8L water bottle)
put a straw for the mouse to walk on there
it will fall inside and drown trying to jump out
RIP mouse
* DIY trap: with oil:
https://www.youtube.com/watch?v=BxxFNkNf6q8
¶Ants
How to repulse?
* use fire to kill them
* vaccum the ant line
* desinfect to remove traces (if more would follow)
* set a barrier with salt and cinnamon
https://www.toutpratique.com/5-La-maison/69-La-lutte-anti-acarien-et-la-lutte-anti-insectes-cafards-mites-punaises-etc-/4741-les-fourmis-quoi-faire-contre-les-fourmis-a-la-maison.php
--------------
next time:
* try BORAX (acid)?:
https://www.amazon.fr/KB-HOME-DEFENSE-Fourmis-Boite/dp/B073FFM49F
* [...]
Biting ants?
... depends on the type!
____________________________
Log:
1) invasion in house @Paillard
* check where they enter <- window
* they are attracted by food, remove food <- not in this case
2) (20200511 @ jablito.fuertventura):
possible invasion by "Carpenter Ants"...:
https://en.wikipedia.org/wiki/Carpenter_ant
"""Carpenter ants are one of the largest of all ant species. Carpenter ants have polymorphic workers, meaning that ants within a single colony may vary in size. Adult carpenter ants can measure from 6 to 12 mm in length. Males, or winged swarmers, can measure up to 18 mm, while queens grow to 20 mm in length."""
https://www.orkin.com/ants/carpenter-ant/carpenter-ant-size
How to repulse?
* use fire to kill them
* vaccum the ant line
* desinfect to remove traces (if more would follow)
* set a barrier with salt and cinnamon
https://www.toutpratique.com/5-La-maison/69-La-lutte-anti-acarien-et-la-lutte-anti-insectes-cafards-mites-punaises-etc-/4741-les-fourmis-quoi-faire-contre-les-fourmis-a-la-maison.php
--------------
next time:
* try BORAX (acid)?:
https://www.amazon.fr/KB-HOME-DEFENSE-Fourmis-Boite/dp/B073FFM49F
* [...]
Biting ants?
... depends on the type!
____________________________
Log:
1) invasion in house @Paillard
* check where they enter <- window
* they are attracted by food, remove food <- not in this case
2) (20200511 @ jablito.fuertventura):
possible invasion by "Carpenter Ants"...:
https://en.wikipedia.org/wiki/Carpenter_ant
"""Carpenter ants are one of the largest of all ant species. Carpenter ants have polymorphic workers, meaning that ants within a single colony may vary in size. Adult carpenter ants can measure from 6 to 12 mm in length. Males, or winged swarmers, can measure up to 18 mm, while queens grow to 20 mm in length."""
https://www.orkin.com/ants/carpenter-ant/carpenter-ant-size
¶Cats
→ 🔗postcats
### tomerge !!!
* they piss on your stuff
* they bring you fleas
* they give you 🔗toxoplasmosis
* they break your garbage in search for food
* they steal your fish
* [...]
How to repulse?
Dislike certain odors:
* lemon & orange peels
* wet coffee
* minth
* lavender
Check also:
* https://www.alleycat.org/resources/how-to-live-with-cats-in-your-neighborhood/
* https://www.easyologypets.com/blogs/news/smells-cats-hate
→ 🔗postcats
* they piss on your stuff
* they bring you fleas
* they give you 🔗toxoplasmosis
* they break your garbage in search for food
* [...]
How to repulse?
Dislike certain odors:
* lemon & orange peels
* wet coffee
* minth
* lavender
Check also:
* https://www.alleycat.org/resources/how-to-live-with-cats-in-your-neighborhood/
* https://www.easyologypets.com/blogs/news/smells-cats-hate
¶Cockroaches
esp: "Cucaracha"
Tips:
* Always turn around your shoes!
* They will hide in anything you leave outside even for seconds:
shopping bags, boxes, empty trash cans ...
... and so you will bring them in your house
* are also conductive to trapping:
water with bait (rotting fish worked well once!))
* clean house regularly with chlorine/lejia (weekly)
* close all holes in house! (door, etc)
* learn how egg sacks look like
* they like to live inside couches & in dark, moist spots (like back of kitchen closets)
* [...]
Trapping
https://www.wikihow.com/Trap-Cockroaches
______________________
"German cockroaches"
"""
The German cockroach (Blattella germanica), colloquially known as the croton bug, is a species of small cockroach, typically about 1.1 to 1.6 cm (0.43 to 0.63 in)[1][2] long
"""
2022: Found in Kranj, Slovenia
https://njaes.rutgers.edu/fs1322/
________________________________________________
###:
* diseases?
* how to repulse?
* how to detect?
* where will they crawl?:
they didn't get into the van ever (except once when brought in)
so they didn't go up the car? why not?
* [...]
esp: "Cucaracha"
Tips:
* Always turn around your shoes!
* They will hide in anything you leave outside even for seconds:
shopping bags, boxes, empty trash cans ...
... and so you will bring them in your house
* are also conductive to trapping:
water with bait (rotting fish worked well once!))
* clean house regularly with chlorine/lejia (weekly)
* close all holes in house! (door, etc)
* learn how egg sacks look like
* they like to live inside couches & in dark, moist spots (like back of kitchen closets)
* [...]
Trapping
https://www.wikihow.com/Trap-Cockroaches
______________________
"German cockroaches"
"""
The German cockroach (Blattella germanica), colloquially known as the croton bug, is a species of small cockroach, typically about 1.1 to 1.6 cm (0.43 to 0.63 in)[1][2] long
"""
2022: Found in Kranj, Slovenia
https://njaes.rutgers.edu/fs1322/
________________________________________________
###:
* diseases?
* how to repulse?
* how to detect?
* where will they crawl?:
they didn't get into the van ever (except once when brought in)
so they didn't go up the car? why not?
* [...]
¶Termites
(NOT thermites)
CUBA: "comejen"
They are a problem in Canarias!
### wrote about this before #tomerge
Do they bite?:
* "soldier termites", part of the colony, could. but it's unlikely you'll have contact
* [...]
__________ [!!!] CAN THEY TRANSMIT DISEASES? ________
https://www.ibertrac.com/servicios-de-eliminacion-de-plagas/termitas/danos-causan-las-termitas/
"""
No pican ni muerden al ser humano, por lo que no se consideran portadoras de enfermedades, tampoco son conocidas por provocar ningún tipo de alergia, sin embargo ha habido edificios que se han desplomado por su acción afectando gravemente a las personas que había en su interior.
"""
@Cuba, some librarians said so!
(found this at Jose Marti library, the librarian was afraid of them and "### bacteria" they spread)
"we are accustumed, but you ... less ... don't catch some infermedad ..."
https://ortexpest.com/pest/why-you-should-never-ignore-house-termites/
this pages says yes [!!!**]
"""
2 – Termites Carry Dangerous Diseases
Termites are known to carry some dangerous diseases such as typhus, gastroenteritis, dysentery, and polio. The feces of termites are also responsible for asthma and other respiratory diseases.
"""
but maybe is BS?
CUBA: "comejen"
They are a problem in Canarias!
Do they bite?:
* "soldier termites", part of the colony, could. but it's unlikely you'll have contact
* [...]
__________ [!!!] CAN THEY TRANSMIT DISEASES? ________
https://www.ibertrac.com/servicios-de-eliminacion-de-plagas/termitas/danos-causan-las-termitas/
"""
No pican ni muerden al ser humano, por lo que no se consideran portadoras de enfermedades, tampoco son conocidas por provocar ningún tipo de alergia, sin embargo ha habido edificios que se han desplomado por su acción afectando gravemente a las personas que había en su interior.
"""
@Cuba, some librarians said so!
"we are accustumed, but you ... less ... don't catch some infermedad ..."
https://ortexpest.com/pest/why-you-should-never-ignore-house-termites/
this pages says yes [!!!**]
"""
2 – Termites Carry Dangerous Diseases
Termites are known to carry some dangerous diseases such as typhus, gastroenteritis, dysentery, and polio. The feces of termites are also responsible for asthma and other respiratory diseases.
"""
but maybe is BS?
¶Ladybugs
the cuttest insect :D
https://www.thoughtco.com/fascinating-facts-about-ladybugs-1968120
But an invasive species:
https://en.wikipedia.org/wiki/Harmonia_axyridis
"" While predatory species are often used as biological control agents, introduced species of coccinellids are not necessarily benign. Species such as Harmonia axyridis or Coccinella septempunctata in North America outcompete and displace native coccinellids and become pests themselves. ""
STILL THO:
https://fr.wikihow.com/prendre-soin-d%27une-coccinelle
taking care of a ladybug <3
the cuttest insect :D
https://www.thoughtco.com/fascinating-facts-about-ladybugs-1968120
But an invasive species:
https://en.wikipedia.org/wiki/Harmonia_axyridis
"" While predatory species are often used as biological control agents, introduced species of coccinellids are not necessarily benign. Species such as Harmonia axyridis or Coccinella septempunctata in North America outcompete and displace native coccinellids and become pests themselves. ""
STILL THO:
https://fr.wikihow.com/prendre-soin-d%27une-coccinelle
taking care of a ladybug <3
¶(LIST OF LISTS)
#LoL
:
* https://en.wikipedia.org/wiki/Neglected_tropical_diseases
* https://www.orkin.com/other
* https://en.wikipedia.org/wiki/Neglected_disease
* https://en.wikipedia.org/wiki/Category:Zoonotic_bacterial_diseases
* https://en.wikipedia.org/wiki/Category:Zoonoses
* [...]
:
* https://en.wikipedia.org/wiki/Neglected_tropical_diseases
* https://www.orkin.com/other
* https://en.wikipedia.org/wiki/Neglected_disease
* https://en.wikipedia.org/wiki/Category:Zoonotic_bacterial_diseases
* https://en.wikipedia.org/wiki/Category:Zoonoses
* [...]
¶[!!] SKIN/CONTAGION— Candida (fungal) → candidiasis, especially Candida auris
https://www.healthline.com/nutrition/candida-symptoms-treatment#section8
"""
A Candida yeast infection can also be identified by a KOH test by taking scrapings from the mouth (oral thrush), vagina (vaginitis) and skin (candidiasis). There are over 40 different fungus species known to cause disease in humans, of which Candida albicans is the most common and most frequently tested for.
"""
https://en.wikipedia.org/wiki/Candidiasis
"""
High level Candida colonization is linked to several diseases of the gastrointestinal tract including Crohn's disease.[89][90]
There has been an increase in resistance to antifungals worldwide over the past 30–40 years.[91][92]
"""
https://en.wikipedia.org/wiki/Oral_candidiasis
(==white tongue)
"""
Oral candidiasis, also known as oral thrush among other names,[1] is candidiasis that occurs in the mouth. That is, oral candidiasis is a mycosis (yeast/fungal infection) of Candida species on the mucous membranes of the mouth.
[...]
In humans, oral candidiasis is the most common form of candidiasis,[17] by far the most common fungal infection of the mouth,[5] and it also represents the most common opportunistic oral infection in humans[40] with lesions only occurring when the environment favors pathogenic behavior.
"""
________________
https://en.wikipedia.org/wiki/Invasive_candidiasis
"""
Invasive candidiasis is caused by 15 of the more than 150 known species of Candida. These species, all confirmed by isolation from patients, are: C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, C. krusei, C. guilliermondii, C. lusitaniae, C. dubliniensis, C. pelliculosa, C. kefyr, C. lipolytica, C. famata, C. inconspicua, C. rugosa, and C. norvegensis.[4] Over the last 20–30 years, C. albicans has been responsible for 95% of infections, with, C. glabrata, C. parapsilosis, C. tropicalis, and C. krusei causing the majority of the remaining cases.[4] Recently, C. auris, a species first reported in 2009, has been found to cause invasive candidiasis. C. auris has attracted attention because it can be resistant to the antifungal medications used to treat candidiasis.[5]
"""
""""
Candida auris is an emerging multidrug-resistant yeast that can cause invasive candidiasis and is associated with high mortality.[6] It was first described in 2009.[6] Since then, C. auris infections, specifically fungemia, have been reported from South Korea, India, South Africa, Kuwait, Colombia, Venezuela, Pakistan, the United Kingdom and the United States.[6] The strains isolated in each region are genetically distinct, indicating that this species is emerging in different locations.[6] The reason for this pattern is unknown.[6]
"""
(difficult diagnosis)
"""
Positive culture of Candida species from normally sterile sites, such as blood, cerebrospinal fluid, pericardium, pericardial fluid, or biopsied tissue, is definitive evidence of invasive candidiasis.[2] Diagnosis by culturing allows subsequent susceptibility testing of causative species.[8][7] Sensitivity of blood culture is far from ideal, with a sensitivity reported to be between 21 and 71%
""
(treatment)
"""
Antifungals are used for treatment with the specific type and dose depending on the patient's age, immune status, and specifics of the infection. For most adults, the initial treatment is an echinocandin class antifungal (caspofungin, micafungin, or anidulafungin) given intravenously. Fluconazole, amphotericin B, and other antifungals may also be used
"""
_________
https://en.wikipedia.org/wiki/Candida_tropicalis
"""
In tropical countries, C. tropicalis is one of the most common colonizer and pathogen causing human disease,[5] especially found on human skin, in the gastrointestinal tract and also in female genitourinary tract.[4] It can be transmitted between health-care workers and patients,[5] especially in environments such as hospitals.[5] C. tropicalis can survive for up to 24 hours therefore be cross-transmitted to a second hand with a probability of 69% and to a third hand with 38% probability.[5] It is the cause responsible for approximately half of the beyond-surface candida infections.[5] C. tropicalis is the second most virulent Candida species[7] that can significantly affect by spreading through the weakened immune system host and can occupy the gastrointestinal tract within 30 minutes of inoculation, all this resulting in increased mortality.[5][14][10] Impact of candidiasis, infections cause by C. tropicalis, have increased globally.[14] C. tropicalis is virulent due to its ability to produce biofilm, secrete lytic enzymes, adhere to epithelial and endothelial cells, and undergo transition of bud to hyphae.[15][10][7]
"""
https://www.healthline.com/nutrition/candida-symptoms-treatment#section8
"""
A Candida yeast infection can also be identified by a KOH test by taking scrapings from the mouth (oral thrush), vagina (vaginitis) and skin (candidiasis). There are over 40 different fungus species known to cause disease in humans, of which Candida albicans is the most common and most frequently tested for.
"""
https://en.wikipedia.org/wiki/Candidiasis
"""
High level Candida colonization is linked to several diseases of the gastrointestinal tract including Crohn's disease.[89][90]
There has been an increase in resistance to antifungals worldwide over the past 30–40 years.[91][92]
"""
https://en.wikipedia.org/wiki/Oral_candidiasis
(==white tongue)
"""
Oral candidiasis, also known as oral thrush among other names,[1] is candidiasis that occurs in the mouth. That is, oral candidiasis is a mycosis (yeast/fungal infection) of Candida species on the mucous membranes of the mouth.
[...]
In humans, oral candidiasis is the most common form of candidiasis,[17] by far the most common fungal infection of the mouth,[5] and it also represents the most common opportunistic oral infection in humans[40] with lesions only occurring when the environment favors pathogenic behavior.
"""
________________
https://en.wikipedia.org/wiki/Invasive_candidiasis
"""
Invasive candidiasis is caused by 15 of the more than 150 known species of Candida. These species, all confirmed by isolation from patients, are: C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, C. krusei, C. guilliermondii, C. lusitaniae, C. dubliniensis, C. pelliculosa, C. kefyr, C. lipolytica, C. famata, C. inconspicua, C. rugosa, and C. norvegensis.[4] Over the last 20–30 years, C. albicans has been responsible for 95% of infections, with, C. glabrata, C. parapsilosis, C. tropicalis, and C. krusei causing the majority of the remaining cases.[4] Recently, C. auris, a species first reported in 2009, has been found to cause invasive candidiasis. C. auris has attracted attention because it can be resistant to the antifungal medications used to treat candidiasis.[5]
"""
""""
Candida auris is an emerging multidrug-resistant yeast that can cause invasive candidiasis and is associated with high mortality.[6] It was first described in 2009.[6] Since then, C. auris infections, specifically fungemia, have been reported from South Korea, India, South Africa, Kuwait, Colombia, Venezuela, Pakistan, the United Kingdom and the United States.[6] The strains isolated in each region are genetically distinct, indicating that this species is emerging in different locations.[6] The reason for this pattern is unknown.[6]
"""
(difficult diagnosis)
"""
Positive culture of Candida species from normally sterile sites, such as blood, cerebrospinal fluid, pericardium, pericardial fluid, or biopsied tissue, is definitive evidence of invasive candidiasis.[2] Diagnosis by culturing allows subsequent susceptibility testing of causative species.[8][7] Sensitivity of blood culture is far from ideal, with a sensitivity reported to be between 21 and 71%
""
(treatment)
"""
Antifungals are used for treatment with the specific type and dose depending on the patient's age, immune status, and specifics of the infection. For most adults, the initial treatment is an echinocandin class antifungal (caspofungin, micafungin, or anidulafungin) given intravenously. Fluconazole, amphotericin B, and other antifungals may also be used
"""
_________
https://en.wikipedia.org/wiki/Candida_tropicalis
"""
In tropical countries, C. tropicalis is one of the most common colonizer and pathogen causing human disease,[5] especially found on human skin, in the gastrointestinal tract and also in female genitourinary tract.[4] It can be transmitted between health-care workers and patients,[5] especially in environments such as hospitals.[5] C. tropicalis can survive for up to 24 hours therefore be cross-transmitted to a second hand with a probability of 69% and to a third hand with 38% probability.[5] It is the cause responsible for approximately half of the beyond-surface candida infections.[5] C. tropicalis is the second most virulent Candida species[7] that can significantly affect by spreading through the weakened immune system host and can occupy the gastrointestinal tract within 30 minutes of inoculation, all this resulting in increased mortality.[5][14][10] Impact of candidiasis, infections cause by C. tropicalis, have increased globally.[14] C. tropicalis is virulent due to its ability to produce biofilm, secrete lytic enzymes, adhere to epithelial and endothelial cells, and undergo transition of bud to hyphae.[15][10][7]
"""
¶SKIN/CONTAGION— Streptococcus (bacterial)
https://dermnetnz.org/topics/streptococcal-skin-infections/
"""
In addition, streptococci are capable of causing skin disease through means other than direct infection of the skin; for example:
https://dermnetnz.org/topics/streptococcal-skin-infections/
"""
In addition, streptococci are capable of causing skin disease through means other than direct infection of the skin; for example:
- Scarlet fever is a reaction to a circulating toxin that is produced by some strains of streptococcus
- Streptococcal toxic shock-like syndrome (STSS)
- Allergic hypersensitivity to streptococcal bacteria may result in erythema nodosum or vasculitis
- Psoriasis, especially guttate forms, may be provoked or aggravated by streptococcal infection
- Pustulosis acuta generalisata: scattered sterile pustules on hands, feet and elsewhere following an streptococcal upper respiratory tract infection; may be associated with painful joints.
¶SKIN/CONTAGION— (more: "cysts, lumps and bumps")
https://www.webmd.com/skin-problems-and-treatments/guide/cysts-lumps-bumps#1
https://www.webmd.com/skin-problems-and-treatments/guide/cysts-lumps-bumps#1
¶lice/(cats→)fleas/mites → Typhus
https://en.wikipedia.org/wiki/Typhus
Still around. Will be back.
2018 in LA.
"""
A person can get typhus by coming in contact with fleas that are infected with the bacteria that cause typhus. Fleas become infected when they bite small animals like rats, opossums, and stray cats. Fleas can then spread the bacteria that cause typhus to other animals and humans.
"""
https://en.wikipedia.org/wiki/Typhus
Still around. Will be back.
2018 in LA.
"""
A person can get typhus by coming in contact with fleas that are infected with the bacteria that cause typhus. Fleas become infected when they bite small animals like rats, opossums, and stray cats. Fleas can then spread the bacteria that cause typhus to other animals and humans.
"""
¶RARE— Lutzomyia flies ("sand flies") → Bacteria → Carrion's Disease
"""
Carrion's disease, also known as bartonellosis, is a disease caused by the blood-borne bacteria, Bartonella bacilliformis. The disease is transmitted by the sand fly species Lutzomyia verracarum, as well as lice and fleas, and is found in areas of Peru, Colombia and Ecuador.[13] The lifecycle of the bacteria within Lutzomyia sand flies remain largely unknown, with speculation that the bacteria are spread between sandflies sharing the same breeding grounds and water supplies. The existence of bartonellosis transmission in areas not inhabited by Lutzomyia verracarum suggests that secondary vectors, and potentially other Lutzomyia species, are important in the spread of the disease.[14]
"""
https://en.wikipedia.org/wiki/Lutzomyia
"""
Carrion's disease, also known as bartonellosis, is a disease caused by the blood-borne bacteria, Bartonella bacilliformis. The disease is transmitted by the sand fly species Lutzomyia verracarum, as well as lice and fleas, and is found in areas of Peru, Colombia and Ecuador.[13] The lifecycle of the bacteria within Lutzomyia sand flies remain largely unknown, with speculation that the bacteria are spread between sandflies sharing the same breeding grounds and water supplies. The existence of bartonellosis transmission in areas not inhabited by Lutzomyia verracarum suggests that secondary vectors, and potentially other Lutzomyia species, are important in the spread of the disease.[14]
"""
https://en.wikipedia.org/wiki/Lutzomyia
¶PINWORMS → itching anus
https://en.wikipedia.org/wiki/Pinworm_infection
https://kidspluspgh.com/doctors-notes/lice-scabies-pinworms/
Diagnosis → https://www.cdc.gov/parasites/pinworm/diagnosis.html
https://en.wikipedia.org/wiki/Pinworm_infection
https://kidspluspgh.com/doctors-notes/lice-scabies-pinworms/
Diagnosis → https://www.cdc.gov/parasites/pinworm/diagnosis.html
¶TRIATOMINE bugs → T. cruzi → CHAGAS DISEASE
aaaaaaaaaaaa
@south.america
"""
T. cruzi
This parasite causes Chagas disease, which can be life-threatening. People get infected from contact with the bug’s feces. Symptoms show up quickly as fever, fatigue, aches, headache, rash, loss of appetite, diarrhea, vomiting, and swollen eyelids. Later, it can lead to heart and intestine problems. Doctors treat the disease and kill the parasite with medication.
"""
here: ??????
The triatomine bugs are capable of colonizing poorly constructed homes in rural, suburban and urban areas
Triatomine bugs can infect rodent, marsupials and other wild mammals. These triatomine bugs can also infect domesticated animals such as dogs and cat, and bring the T. cruzi (agent of the disease) inside human dwellings.
* fuck this is horrible https://www.paho.org/hq/index.php?option=com_content&view=article&id=5856:2011-informacion-general-enfermedad-chagas&Itemid=40370&lang=en
"""
Triatominae
"""
more:
* https://www.cdc.gov/parasites/chagas/gen_info/detailed.html
* https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008404 :
"Fast recovery of house infestation with Triatoma brasiliensis after residual insecticide spraying in a semiarid region of Northeastern Brazil"
* [...]
aaaaaaaaaaaa
@south.america
"""
T. cruzi
This parasite causes Chagas disease, which can be life-threatening. People get infected from contact with the bug’s feces. Symptoms show up quickly as fever, fatigue, aches, headache, rash, loss of appetite, diarrhea, vomiting, and swollen eyelids. Later, it can lead to heart and intestine problems. Doctors treat the disease and kill the parasite with medication.
"""
here: ??????
The triatomine bugs are capable of colonizing poorly constructed homes in rural, suburban and urban areas
Triatomine bugs can infect rodent, marsupials and other wild mammals. These triatomine bugs can also infect domesticated animals such as dogs and cat, and bring the T. cruzi (agent of the disease) inside human dwellings.
* fuck this is horrible https://www.paho.org/hq/index.php?option=com_content&view=article&id=5856:2011-informacion-general-enfermedad-chagas&Itemid=40370&lang=en
"""
Triatominae
- This nocturnal insect (also known as the kissing bug, 'vinchuca' in Spanish, or 'barbeiro' in Portuguese) is responsible for Chagas in the USA, Mexico, Central America and South America. Sleep under an insecticide-treated bed net.
"""
more:
* https://www.cdc.gov/parasites/chagas/gen_info/detailed.html
* https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008404 :
"Fast recovery of house infestation with Triatoma brasiliensis after residual insecticide spraying in a semiarid region of Northeastern Brazil"
* [...]
¶ [!!**] general test??
Q: How to get tested? How to do a big regular check that includes this kind of shit ???
Q: How to get tested? How to do a big regular check that includes this kind of shit ???
¶ (references/resources)
https://www.webmd.com/skin-problems-and-treatments/ss/slideshow-pictures-of-parasites
https://en.wikipedia.org/wiki/List_of_parasites_of_humans [m!!**]
https://www.webmd.com/skin-problems-and-treatments/ss/slideshow-pictures-of-parasites
https://en.wikipedia.org/wiki/List_of_parasites_of_humans [m!!**]
¶ pork tapeworms → taeniasis & cysticercosis
more:
* https://www.cdc.gov/parasites/taeniasis/gen_info/faqs.html
* https://www.who.int/taeniasis/disease/en/
scarce in "developed" world:
### !!! figure out how to talk about this
"""
T. solium taeniasis/cysticercosis mainly affects the health and livelihoods of subsistence farming communities in developing countries of Africa, Asia and Latin America. It is common in areas where animal husbandry practices are such that pigs and cattle come into contact with human faeces. But imported taeniasis can also lead to cases in the population of countries where T. solium is not considered a public health problem.
"""
_____________
"""They infect the intestines and brain, which can lead to a disease that causes headaches and seizures, called cysticercosis"""
f00k
"""
Cysticercosis is acquired when worm proglottids or eggs are ingested and the developing larvae migrate through the body and form cysts in tissues. This is the case in pigs and cattle but it can also affect humans, usually when they swallow T. solium egg-contaminated soil, water or food (mainly vegetables) or through self-infection when hygiene practices, such as hand washing after the toilet, are unsufficient. When the central nervous system is affected by the larvae, the infection is called neurocysticercosis.
"""
_____________
"""
Humans can become infected with these tapeworms by eating raw or undercooked beef (T. saginata) or pork (T. solium and T. asiatica). People with taeniasis may not know they have a tapeworm infection because symptoms are usually mild or nonexistent.
"""
more:
* https://www.cdc.gov/parasites/taeniasis/gen_info/faqs.html
* https://www.who.int/taeniasis/disease/en/
scarce in "developed" world:
"""
T. solium taeniasis/cysticercosis mainly affects the health and livelihoods of subsistence farming communities in developing countries of Africa, Asia and Latin America. It is common in areas where animal husbandry practices are such that pigs and cattle come into contact with human faeces. But imported taeniasis can also lead to cases in the population of countries where T. solium is not considered a public health problem.
"""
_____________
"""They infect the intestines and brain, which can lead to a disease that causes headaches and seizures, called cysticercosis"""
f00k
"""
Cysticercosis is acquired when worm proglottids or eggs are ingested and the developing larvae migrate through the body and form cysts in tissues. This is the case in pigs and cattle but it can also affect humans, usually when they swallow T. solium egg-contaminated soil, water or food (mainly vegetables) or through self-infection when hygiene practices, such as hand washing after the toilet, are unsufficient. When the central nervous system is affected by the larvae, the infection is called neurocysticercosis.
"""
_____________
"""
Humans can become infected with these tapeworms by eating raw or undercooked beef (T. saginata) or pork (T. solium and T. asiatica). People with taeniasis may not know they have a tapeworm infection because symptoms are usually mild or nonexistent.
"""
¶ Brain-Eating Amoeba (N. fowleri)
wtf
"""
People in the U.S. don’t have to worry as much about this parasite as people in Southeast Asia do. The bug, also known as N. fowleri
"""
↓
so ... not in the west
wtf
"""
People in the U.S. don’t have to worry as much about this parasite as people in Southeast Asia do. The bug, also known as N. fowleri
"""
↓
so ... not in the west
¶ (Roundworms)
"""
Most of these bugs infect your intestines. But the one that causes trichinosis also affects your muscles.
Common roundworm diseases and their symptoms include:
• Ascariasis -- belly pain
• Hookworm -- blood loss
• Pinworm -- anal itching
• Trichinosis -- pain, fever, face swelling, pink eye, rash
• Whipworm -- mucus, water and blood in stool, rectal prolapse (when part or all of the rectum slides out of place)
"""
https://en.wikipedia.org/wiki/Nematode#Parasitic_species
"""
Nematodes that commonly parasitise humans include ascarids (Ascaris), filarias, hookworms, pinworms (Enterobius), and whipworms (Trichuris trichiura). The species Trichinella spiralis, commonly known as the 'trichina worm', occurs in rats, pigs, bears, and humans, and is responsible for the disease trichinosis. Baylisascaris usually infests wild animals, but can be deadly to humans, as well. Dirofilaria immitis is known for causing heartworm disease by inhabiting the hearts, arteries, and lungs of dogs and some cats. Haemonchus contortus is one of the most abundant infectious agents in sheep around the world, causing great economic damage to sheep.
"""
https://en.wikipedia.org/wiki/Ascarididae
https://en.wikipedia.org/wiki/Filarioidea
https://en.wikipedia.org/wiki/Hookworm
https://en.wikipedia.org/wiki/Pinworm_(parasite)
https://en.wikipedia.org/wiki/Trichuris_trichiura
https://en.wikipedia.org/wiki/Trichinella_spiralis
https://en.wikipedia.org/wiki/Baylisascaris
"""
Most of these bugs infect your intestines. But the one that causes trichinosis also affects your muscles.
Common roundworm diseases and their symptoms include:
• Ascariasis -- belly pain
• Hookworm -- blood loss
• Pinworm -- anal itching
• Trichinosis -- pain, fever, face swelling, pink eye, rash
• Whipworm -- mucus, water and blood in stool, rectal prolapse (when part or all of the rectum slides out of place)
"""
https://en.wikipedia.org/wiki/Nematode#Parasitic_species
"""
Nematodes that commonly parasitise humans include ascarids (Ascaris), filarias, hookworms, pinworms (Enterobius), and whipworms (Trichuris trichiura). The species Trichinella spiralis, commonly known as the 'trichina worm', occurs in rats, pigs, bears, and humans, and is responsible for the disease trichinosis. Baylisascaris usually infests wild animals, but can be deadly to humans, as well. Dirofilaria immitis is known for causing heartworm disease by inhabiting the hearts, arteries, and lungs of dogs and some cats. Haemonchus contortus is one of the most abundant infectious agents in sheep around the world, causing great economic damage to sheep.
"""
https://en.wikipedia.org/wiki/Ascarididae
https://en.wikipedia.org/wiki/Filarioidea
https://en.wikipedia.org/wiki/Hookworm
https://en.wikipedia.org/wiki/Pinworm_(parasite)
https://en.wikipedia.org/wiki/Trichuris_trichiura
https://en.wikipedia.org/wiki/Trichinella_spiralis
https://en.wikipedia.org/wiki/Baylisascaris
¶ (dog →) D. immitis / D. repens / D. tenuis → (mosquitos → ) dog/cat/~humans
(roundworm parasite, via mosquitos, via dogs, causing heart fibrosis)
https://en.wikipedia.org/wiki/Dirofilaria_immitis (dog heartworm, also cats, via mosquitos):
"is a parasitic roundworm that is a type of filarial worm, a small thread-like worm, that causes dirofilariasis.
It is spread from host to host through the bites of mosquitoes"
In humans?:
... "RARE" ?!?!
... so, yes.
→ https://en.wikipedia.org/wiki/Dirofilaria_immitis#Heartworm_infection_in_humans
#anticats #antipets
"""
It was thought to infect the human eye, with most cases reported from the southeastern United States. However, these cases are now thought to be caused by a closely related parasite of raccoons, Dirofilaria tenuis. Several hundred cases of subcutaneous infections in humans have been reported in Europe, but these are almost always caused by another closely related parasite, Dirofilaria repens, rather than the dog heartworm. There are proven D. immitis infections,[16] but humans rarely get infected with heartworms due to the larvae never fully maturing
"""
https://en.wikipedia.org/wiki/Dirofilaria_tenuis → (mosquitos→) racoons/~~people
"""
D. tenuis is not compatible with a human host, so it dies much more quickly, living only a few months.
During this time, a lump or nodule will form where the worm is located. This most commonly occurs near the site of the mosquito bite, but can also be much farther away.[9]
D. tenuis may migrate using the host’s blood, leaving the worm anywhere in the body,
even the conjunctiva of the eye.[7]
As the body attempts to clear the worm, the nodule may become painful:
If the patient continues to experience discomfort, the worm may be surgically excised.
Excision is a curative treatment and the worm is diagnosed as D. tenuis easily using its unique morphology.[9]
"""
---------------------
learn to diagnose & operate this kind of shit
#medical #surgery #diy
[→→!!!]
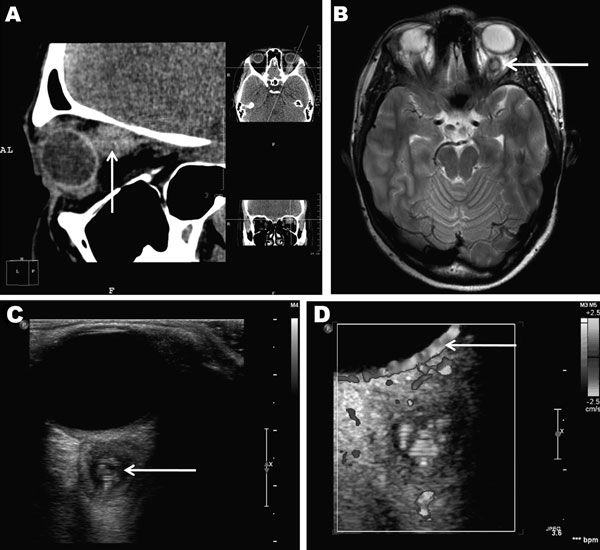
D.repens cyst in 20-year old woman
https://en.wikipedia.org/wiki/Dirofilaria_repens#Infections_in_humans
"""
Although humans may become infected as aberrant hosts, the worms fail to reach adulthood while infecting a human body.
"""
(roundworm parasite, via mosquitos, via dogs, causing heart fibrosis)
https://en.wikipedia.org/wiki/Dirofilaria_immitis (dog heartworm, also cats, via mosquitos):
"is a parasitic roundworm that is a type of filarial worm, a small thread-like worm, that causes dirofilariasis.
It is spread from host to host through the bites of mosquitoes"
In humans?:
... "RARE" ?!?!
... so, yes.
→ https://en.wikipedia.org/wiki/Dirofilaria_immitis#Heartworm_infection_in_humans
#anticats #antipets
"""
It was thought to infect the human eye, with most cases reported from the southeastern United States. However, these cases are now thought to be caused by a closely related parasite of raccoons, Dirofilaria tenuis. Several hundred cases of subcutaneous infections in humans have been reported in Europe, but these are almost always caused by another closely related parasite, Dirofilaria repens, rather than the dog heartworm. There are proven D. immitis infections,[16] but humans rarely get infected with heartworms due to the larvae never fully maturing
"""
https://en.wikipedia.org/wiki/Dirofilaria_tenuis → (mosquitos→) racoons/~~people
"""
D. tenuis is not compatible with a human host, so it dies much more quickly, living only a few months.
During this time, a lump or nodule will form where the worm is located. This most commonly occurs near the site of the mosquito bite, but can also be much farther away.[9]
D. tenuis may migrate using the host’s blood, leaving the worm anywhere in the body,
even the conjunctiva of the eye.[7]
As the body attempts to clear the worm, the nodule may become painful:
If the patient continues to experience discomfort, the worm may be surgically excised.
Excision is a curative treatment and the worm is diagnosed as D. tenuis easily using its unique morphology.[9]
"""
---------------------
learn to diagnose & operate this kind of shit
#medical #surgery #diy
[→→!!!]
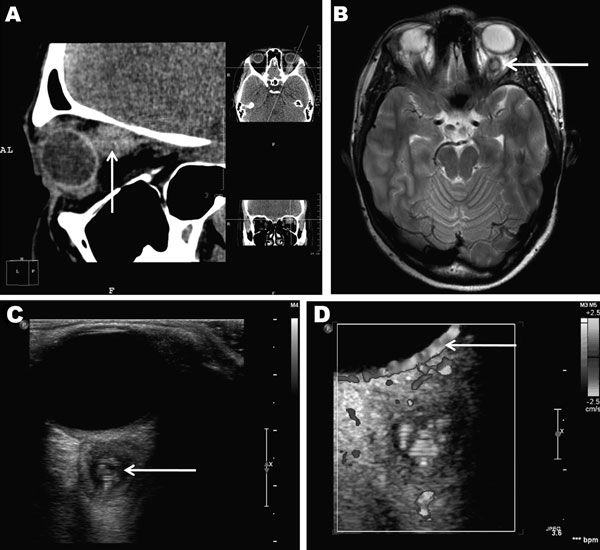
D.repens cyst in 20-year old woman
https://en.wikipedia.org/wiki/Dirofilaria_repens#Infections_in_humans
"""
Although humans may become infected as aberrant hosts, the worms fail to reach adulthood while infecting a human body.
"""
¶ Giardia → diarrhea, etc
!!! might be more common? how to mark?
"""
If you’ve ever been camping and you came down with diarrhea, gas, stomach cramps, bloating, and nausea, you’ve likely caught this bug. You get it through food or drinking water, or from contact with the feces of an infected person or animal. The illness can be treated with prescription drugs.
"""
____________-
"""
Giardiasis is a parasitic disease caused by Giardia duodenalis (also known as G. lamblia and G. intestinalis).[3] Infected individuals who experience symptoms (about 10% have no symptoms) may have diarrhea, abdominal pain, and weight loss.[1] Less common symptoms include vomiting and blood in the stool.[1] Symptoms usually begin 1 to 3 weeks after exposure and, without treatment, may last two to six weeks or longer.[4]
Giardiasis usually spreads when Giardia duodenalis cysts within feces contaminate food or water that is later consumed orally.[1] The disease can also spread between people and through other animals.[1] Cysts may survive for nearly three months in cold water.[1] Giardiasis is diagnosed via stool tests.[1]
[...]
Risk factors include travel in the developing world, changing diapers, eating food without cooking it, and owning a dog.[1] Cysts may survive for nearly three months in cold water.[1] Diagnosis is via stool tests
[...]
Giardia is one of the most common parasitic human diseases globally.[4] In 2013, there were about 280 million people worldwide with symptomatic giardiasis.[4] Rates are as high as 7% in the developed world and 30% in the developing world.[1] The World Health Organization classified it as a neglected disease.[1]
"""
https://en.wikipedia.org/wiki/Giardiasis
"""
If you’ve ever been camping and you came down with diarrhea, gas, stomach cramps, bloating, and nausea, you’ve likely caught this bug. You get it through food or drinking water, or from contact with the feces of an infected person or animal. The illness can be treated with prescription drugs.
"""
____________-
"""
Giardiasis is a parasitic disease caused by Giardia duodenalis (also known as G. lamblia and G. intestinalis).[3] Infected individuals who experience symptoms (about 10% have no symptoms) may have diarrhea, abdominal pain, and weight loss.[1] Less common symptoms include vomiting and blood in the stool.[1] Symptoms usually begin 1 to 3 weeks after exposure and, without treatment, may last two to six weeks or longer.[4]
Giardiasis usually spreads when Giardia duodenalis cysts within feces contaminate food or water that is later consumed orally.[1] The disease can also spread between people and through other animals.[1] Cysts may survive for nearly three months in cold water.[1] Giardiasis is diagnosed via stool tests.[1]
[...]
Risk factors include travel in the developing world, changing diapers, eating food without cooking it, and owning a dog.[1] Cysts may survive for nearly three months in cold water.[1] Diagnosis is via stool tests
[...]
Giardia is one of the most common parasitic human diseases globally.[4] In 2013, there were about 280 million people worldwide with symptomatic giardiasis.[4] Rates are as high as 7% in the developed world and 30% in the developing world.[1] The World Health Organization classified it as a neglected disease.[1]
"""
https://en.wikipedia.org/wiki/Giardiasis
¶ Cryptosporidium
"""
This bug's also called "crypto," and it affects your intestines. It’s spread by contact with the stool of an infected person or animal. People tend to catch it from pool water, especially kids. The diarrhea it causes can last a long time, but it usually goes away on its own without treatment.
"""
"""
This bug's also called "crypto," and it affects your intestines. It’s spread by contact with the stool of an infected person or animal. People tend to catch it from pool water, especially kids. The diarrhea it causes can last a long time, but it usually goes away on its own without treatment.
"""
¶ T. Vaginalis → trichomoniasis STD
"""
This parasite causes a sexually transmitted disease called trichomoniasis, the most common curable STD. Most infected people don’t have any symptoms, but some may notice itching, burning, or irritation of their penis or vagina. It’s treated with antibiotics.
"""
___________________
https://pubmed.ncbi.nlm.nih.gov/1736479/
Sexually transmitted protozoal infections. Trichomonas vaginalis, Entamoeba histolytica, and Giardia lamblia
"""
Collectively, protozoa account for the largest number of STDs worldwide. Although these organisms can be eradicated effectively in the individual patient, their high asymptomatic carriage rate appears to have a significant influence on their continued transmission. The best hope for eradication of these organisms lies in a high index of suspicion in high-risk populations and the careful evaluation and treatment of sexual partners of infected persons.
"""
"""
This parasite causes a sexually transmitted disease called trichomoniasis, the most common curable STD. Most infected people don’t have any symptoms, but some may notice itching, burning, or irritation of their penis or vagina. It’s treated with antibiotics.
"""
___________________
https://pubmed.ncbi.nlm.nih.gov/1736479/
Sexually transmitted protozoal infections. Trichomonas vaginalis, Entamoeba histolytica, and Giardia lamblia
"""
Collectively, protozoa account for the largest number of STDs worldwide. Although these organisms can be eradicated effectively in the individual patient, their high asymptomatic carriage rate appears to have a significant influence on their continued transmission. The best hope for eradication of these organisms lies in a high index of suspicion in high-risk populations and the careful evaluation and treatment of sexual partners of infected persons.
"""
¶ Entamoeba histolytica (STD)
"""
Entamoeba histolytica is an anaerobic parasitic amoebozoan, part of the genus Entamoeba.[1] Predominantly infecting humans and other primates causing amoebiasis, E. histolytica is estimated to infect about 35-50 million people worldwide.[1] E. histolytica infection is estimated to kill more than 55,000 people each year.[2] Previously, it was thought that 10% of the world population was infected, but these figures predate the recognition that at least 90% of these infections were due to a second species, E. dispar.[3] Mammals such as dogs and cats can become infected transiently, but are not thought to contribute significantly to transmission.
[...]
The active (trophozoite) stage exists only in the host and in fresh loose feces; cysts survive outside the host in water, in soils, and on foods, especially under moist conditions on the latter. The infection can occur when a person puts anything into their mouth that has touched the feces of a person who is infected with E. histolytica, swallows something, such as water or food, that is contaminated with E. histolytica, or swallows E. histolytica cysts (eggs) picked up from contaminated surfaces or fingers.[4] The cysts are readily killed by heat and by freezing temperatures; they survive for only a few months outside of the host.[5] When cysts are swallowed, they cause infections by excysting (releasing the trophozoite stage) in the digestive tract.
[...]
Symptoms can include fulminating dysentery, bloody diarrhea, weight loss, fatigue, abdominal pain, and amoeboma. The amoeba can 'bore' into the intestinal wall, causing lesions and intestinal symptoms, and it may reach the bloodstream or peritoneal cavity.[8] From there, it can reach vital organs of the human body, usually the liver, but sometimes the lungs, brain, and spleen.[9] A common outcome of this invasion of tissues is a liver abscess, which can be fatal if untreated
[...]
E. histolytica is also recognized as an emerging sexually transmissible pathogen, especially in male homosexual relations, causing outbreaks in non-endemic regions
"""
TREATMENT
"""
Usually nitroimidazole derivatives (such as metronidazole) are used, because they are highly effective against the trophozoite form of the amoeba.
Since they have little effect on amoeba cysts, usually this treatment is followed by an agent (such as paromomycin or diloxanide furoate) that acts on the organism in the lumen.[2]
"""
"""
Entamoeba histolytica is an anaerobic parasitic amoebozoan, part of the genus Entamoeba.[1] Predominantly infecting humans and other primates causing amoebiasis, E. histolytica is estimated to infect about 35-50 million people worldwide.[1] E. histolytica infection is estimated to kill more than 55,000 people each year.[2] Previously, it was thought that 10% of the world population was infected, but these figures predate the recognition that at least 90% of these infections were due to a second species, E. dispar.[3] Mammals such as dogs and cats can become infected transiently, but are not thought to contribute significantly to transmission.
[...]
The active (trophozoite) stage exists only in the host and in fresh loose feces; cysts survive outside the host in water, in soils, and on foods, especially under moist conditions on the latter. The infection can occur when a person puts anything into their mouth that has touched the feces of a person who is infected with E. histolytica, swallows something, such as water or food, that is contaminated with E. histolytica, or swallows E. histolytica cysts (eggs) picked up from contaminated surfaces or fingers.[4] The cysts are readily killed by heat and by freezing temperatures; they survive for only a few months outside of the host.[5] When cysts are swallowed, they cause infections by excysting (releasing the trophozoite stage) in the digestive tract.
[...]
Symptoms can include fulminating dysentery, bloody diarrhea, weight loss, fatigue, abdominal pain, and amoeboma. The amoeba can 'bore' into the intestinal wall, causing lesions and intestinal symptoms, and it may reach the bloodstream or peritoneal cavity.[8] From there, it can reach vital organs of the human body, usually the liver, but sometimes the lungs, brain, and spleen.[9] A common outcome of this invasion of tissues is a liver abscess, which can be fatal if untreated
[...]
E. histolytica is also recognized as an emerging sexually transmissible pathogen, especially in male homosexual relations, causing outbreaks in non-endemic regions
"""
TREATMENT
"""
Usually nitroimidazole derivatives (such as metronidazole) are used, because they are highly effective against the trophozoite form of the amoeba.
Since they have little effect on amoeba cysts, usually this treatment is followed by an agent (such as paromomycin or diloxanide furoate) that acts on the organism in the lumen.[2]
"""
¶ Guinea Worm :-o → Dracunculiasis
fuck me
"""
This roundworm's days of spreading disease are nearly done, thanks to health groups that teach people how to avoid getting infected. People catch the bug by drinking water from ponds infected with larvae. The worms mate and grow in the stomach, then burst out through a blister on the skin. Symptoms can include fever, swelling, and pain near the blister, but it usually takes a year after infection for warning signs to show up. There’s no treatment.
"""
https://en.wikipedia.org/wiki/Dracunculiasis
"""
Dracunculiasis, also called Guinea-worm disease, is a parasitic infection by the Guinea worm, Dracunculus medinensis. A person becomes infected by drinking water contaminated with Guinea-worm larvae that reside inside copepods (a type of small crustacean). Stomach acid digests the copepod and releases the Guinea worm, which penetrates the digestive tract and escapes into the body. Around a year later, the adult female migrates to an exit site – usually the lower leg – and induces an intensely painful blister on the skin. Eventually, the blister bursts, creating a painful wound from which the worm gradually emerges over several weeks. The wound remains painful throughout the worm's emergence, disabling the affected person for the three to ten weeks it takes the worm to emerge.
"""
fuck me
"""
This roundworm's days of spreading disease are nearly done, thanks to health groups that teach people how to avoid getting infected. People catch the bug by drinking water from ponds infected with larvae. The worms mate and grow in the stomach, then burst out through a blister on the skin. Symptoms can include fever, swelling, and pain near the blister, but it usually takes a year after infection for warning signs to show up. There’s no treatment.
"""
https://en.wikipedia.org/wiki/Dracunculiasis
"""
Dracunculiasis, also called Guinea-worm disease, is a parasitic infection by the Guinea worm, Dracunculus medinensis. A person becomes infected by drinking water contaminated with Guinea-worm larvae that reside inside copepods (a type of small crustacean). Stomach acid digests the copepod and releases the Guinea worm, which penetrates the digestive tract and escapes into the body. Around a year later, the adult female migrates to an exit site – usually the lower leg – and induces an intensely painful blister on the skin. Eventually, the blister bursts, creating a painful wound from which the worm gradually emerges over several weeks. The wound remains painful throughout the worm's emergence, disabling the affected person for the three to ten weeks it takes the worm to emerge.
"""
¶ (cats → ) Toxoplasma → Toxoplasmosis
#anticats
"""
This bug makes its home in meat, water, and infected cat feces. It causes an illness called toxoplasmosis, which can feel like the flu. Pregnant women and people with weak immune systems can have serious symptoms, like cysts in the muscles, brain, and eyes. Usually it isn’t treated, but a doctor can prescribe medication for a severe infection.
"""
→ 🔗toxoplasmosis
#anticats
"""
This bug makes its home in meat, water, and infected cat feces. It causes an illness called toxoplasmosis, which can feel like the flu. Pregnant women and people with weak immune systems can have serious symptoms, like cysts in the muscles, brain, and eyes. Usually it isn’t treated, but a doctor can prescribe medication for a severe infection.
"""
→ 🔗toxoplasmosis
¶ @sea → parasites → "Swimmer's itch" / cercarial dermatitis
https://www.cdc.gov/parasites/swimmersitch/faqs.html
https://www.mayoclinic.org/diseases-conditions/swimmers-itch/symptoms-causes/syc-20355043
https://en.wikipedia.org/wiki/Swimmer%27s_itch
"""
These parasites are released from infected snails into fresh and salt water (such as lakes, ponds, and oceans).
While the parasite’s preferred host is the specific bird or mammal, if the parasite comes into contact with a swimmer, it burrows into the skin causing an allergic reaction and rash. Swimmer’s itch is found throughout the world and is more frequent during summer months.
"""
"""
The parasites that cause swimmer's itch live in the blood of waterfowl and in mammals that live near ponds and lakes. Examples include:
"""
"""
caused by the larval stage of a group of flatworm parasites in the family Schistosomatidae.[6] The genera most commonly associated with swimmer's itch in humans are Trichobilharzia[1] and Gigantobilharzia. It can also be caused by schistosome parasites of non-avian vertebrates, such as Schistosomatium douthitti, which infects snails and rodents. Other taxa reported to cause the reaction include Bilharziella polonica and Schistosoma bovis. In marine habitats, especially along the coasts, swimmer's itch can occur as well.[7]
"""
https://www.cdc.gov/parasites/swimmersitch/faqs.html
https://www.mayoclinic.org/diseases-conditions/swimmers-itch/symptoms-causes/syc-20355043
https://en.wikipedia.org/wiki/Swimmer%27s_itch
"""
These parasites are released from infected snails into fresh and salt water (such as lakes, ponds, and oceans).
While the parasite’s preferred host is the specific bird or mammal, if the parasite comes into contact with a swimmer, it burrows into the skin causing an allergic reaction and rash. Swimmer’s itch is found throughout the world and is more frequent during summer months.
"""
"""
The parasites that cause swimmer's itch live in the blood of waterfowl and in mammals that live near ponds and lakes. Examples include:
- Geese
- Ducks
- Gulls
- Beavers
- Muskrats
"""
"""
caused by the larval stage of a group of flatworm parasites in the family Schistosomatidae.[6] The genera most commonly associated with swimmer's itch in humans are Trichobilharzia[1] and Gigantobilharzia. It can also be caused by schistosome parasites of non-avian vertebrates, such as Schistosomatium douthitti, which infects snails and rodents. Other taxa reported to cause the reaction include Bilharziella polonica and Schistosoma bovis. In marine habitats, especially along the coasts, swimmer's itch can occur as well.[7]
"""
¶ parasitic flatworms schisotopes → Schistosomiasis
https://en.wikipedia.org/wiki/Schistosomiasis
"""
Schistosomiasis, also known as snail fever and bilharzia,[9] is a disease caused by parasitic flatworms called schistosomes.[5] The urinary tract or the intestines may be infected.[5] Symptoms include abdominal pain, diarrhea, bloody stool, or blood in the urine.[5] Those who have been infected for a long time may experience liver damage, kidney failure, infertility, or bladder cancer.[5] In children, it may cause poor growth and learning difficulty.[5]
[...]
Diagnosis is by finding eggs of the parasite in a person's urine or stool.[5] It can also be confirmed by finding antibodies against the disease in the blood.[5]
[...]
Schistosomiasis affected about 252 million people worldwide in 2015.[6] An estimated 4,400 to 200,000 people die from it each year.[7][8] The disease is most commonly found in Africa, Asia, and South America.[5] Around 700 million people, in more than 70 countries, live in areas where the disease is common
"""
https://en.wikipedia.org/wiki/Schistosomiasis
"""
Schistosomiasis, also known as snail fever and bilharzia,[9] is a disease caused by parasitic flatworms called schistosomes.[5] The urinary tract or the intestines may be infected.[5] Symptoms include abdominal pain, diarrhea, bloody stool, or blood in the urine.[5] Those who have been infected for a long time may experience liver damage, kidney failure, infertility, or bladder cancer.[5] In children, it may cause poor growth and learning difficulty.[5]
[...]
Diagnosis is by finding eggs of the parasite in a person's urine or stool.[5] It can also be confirmed by finding antibodies against the disease in the blood.[5]
[...]
Schistosomiasis affected about 252 million people worldwide in 2015.[6] An estimated 4,400 to 200,000 people die from it each year.[7][8] The disease is most commonly found in Africa, Asia, and South America.[5] Around 700 million people, in more than 70 countries, live in areas where the disease is common
"""
¶ (ocean/water/land) amoeba + contact lenses → acanthamoeba keratitis
https://en.wikipedia.org/wiki/Acanthamoeba_keratitis
"""
In the United States, Acanthamoeba keratitis is nearly always associated with soft contact lens use.[7] Acanthamoeba spp. is most commonly introduced to the eye by contact lenses that have been exposed to the organism through the use of contaminated lens solution, using homemade saline-based solution or tap water, or from wearing contact lenses while bathing or swimming
[...]
Infection of the cornea by Acanthamoeba is difficult to treat with conventional medications, and Acanthamoeba keratitis (AK) may cause permanent visual impairment or blindness, due to damage to the cornea or through damage to other structures important to vision
[...]
Further predisposing factors include contaminated home water supply, and low socioeconomic status. Infection is also more commonly seen in tropical or sub-tropical climates
"""
Diagnosis:
* "ring infiltrate" !!! (~50% cases)
* [!!???]:
* how to self-diagnose?
* how fast does it develop?
* can it easily be told apart from simple contact lense "eye tiredness" or "small conjunctivitis"
* how prevalent is it?
* [...]
also see:
* https://en.wikipedia.org/wiki/Hypopyon
* https://en.wikipedia.org/wiki/Glaucoma
* [...]
https://en.wikipedia.org/wiki/Acanthamoeba_keratitis
"""
In the United States, Acanthamoeba keratitis is nearly always associated with soft contact lens use.[7] Acanthamoeba spp. is most commonly introduced to the eye by contact lenses that have been exposed to the organism through the use of contaminated lens solution, using homemade saline-based solution or tap water, or from wearing contact lenses while bathing or swimming
[...]
Infection of the cornea by Acanthamoeba is difficult to treat with conventional medications, and Acanthamoeba keratitis (AK) may cause permanent visual impairment or blindness, due to damage to the cornea or through damage to other structures important to vision
[...]
Further predisposing factors include contaminated home water supply, and low socioeconomic status. Infection is also more commonly seen in tropical or sub-tropical climates
"""
Diagnosis:
* "ring infiltrate" !!! (~50% cases)
* [!!???]:
* how to self-diagnose?
* how fast does it develop?
* can it easily be told apart from simple contact lense "eye tiredness" or "small conjunctivitis"
* how prevalent is it?
* [...]
also see:
* https://en.wikipedia.org/wiki/Hypopyon
* https://en.wikipedia.org/wiki/Glaucoma
* [...]
¶Fasciolopsis buski
#CONSPIRACY THEORY , CONSIDERED FAKE, BUT INTERESTING
↓↓↓
by https://en.wikipedia.org/wiki/Hulda_Regehr_Clark
"""
In her book The Cure For All Cancers, Clark postulated all cancers and many other diseases are caused by the flatworm Fasciolopsis buski. "The adult [fluke], though, stays tightly stuck to our intestine or liver, causing cancer, or uterus, causing endometriosis, or thymus, causing AIDS, or kidney, causing Hodgkin's disease)."[10] "I have found that cancer, HIV, diabetes, endometriosis, Hodgkin's disease, Alzheimer's disease, lupus, MS and "universal allergy syndrome" are examples of fluke disease."
"""
https://en.wikipedia.org/wiki/Fasciolopsiasis
#CONSPIRACY THEORY , CONSIDERED FAKE, BUT INTERESTING
↓↓↓
by https://en.wikipedia.org/wiki/Hulda_Regehr_Clark
"""
In her book The Cure For All Cancers, Clark postulated all cancers and many other diseases are caused by the flatworm Fasciolopsis buski. "The adult [fluke], though, stays tightly stuck to our intestine or liver, causing cancer, or uterus, causing endometriosis, or thymus, causing AIDS, or kidney, causing Hodgkin's disease)."[10] "I have found that cancer, HIV, diabetes, endometriosis, Hodgkin's disease, Alzheimer's disease, lupus, MS and "universal allergy syndrome" are examples of fluke disease."
"""
https://en.wikipedia.org/wiki/Fasciolopsiasis
¶Dracunculiasis / Guinea-worm disease
https://en.wikipedia.org/wiki/Dracunculiasis
"""
Dracunculiasis, also called Guinea-worm disease, is a parasitic infection by the Guinea worm, Dracunculus medinensis. A person becomes infected from drinking water that contains water fleas infected with guinea worm larvae. After ingestion, the worms penetrate the digestive tract and escape into the body, where they develop over the course of a year. Eventually, the adult worm migrates to an exit site – usually a lower limb – and induces an intensely painful blister on the skin.
"""
almost eradicated!
"""
Previously affecting millions of people across Africa, India, and the Middle East, Guinea worm is now nearly eradicated, with just 27 cases documented in 2020.[3] It will likely be the first parasitic disease to be globally eradicated.[4] Because dogs may also become infected,[5] the eradication program is monitoring and treating dogs as well.[6]
Guinea worm disease has been known since ancient times.
"""
<--------------------- (new) MORE PARASITES
https://en.wikipedia.org/wiki/Dracunculiasis
"""
Dracunculiasis, also called Guinea-worm disease, is a parasitic infection by the Guinea worm, Dracunculus medinensis. A person becomes infected from drinking water that contains water fleas infected with guinea worm larvae. After ingestion, the worms penetrate the digestive tract and escape into the body, where they develop over the course of a year. Eventually, the adult worm migrates to an exit site – usually a lower limb – and induces an intensely painful blister on the skin.
"""
almost eradicated!
"""
Previously affecting millions of people across Africa, India, and the Middle East, Guinea worm is now nearly eradicated, with just 27 cases documented in 2020.[3] It will likely be the first parasitic disease to be globally eradicated.[4] Because dogs may also become infected,[5] the eradication program is monitoring and treating dogs as well.[6]
Guinea worm disease has been known since ancient times.
"""
<--------------------- (new) MORE PARASITES
¶Bacteria+Amoeba symbiosis in water tanks → Legionnaires' disease (pneumonia)
pneumonia caused by contaminated hot water tanks
(for this reason, you need to be careful with hot water installations in unused houses)
https://en.wikipedia.org/wiki/Legionnaires%27_disease
"""
Legionnaires' disease, also known as legionellosis, is a form of atypical pneumonia caused by any type of Legionella bacteria.[3] Signs and symptoms include cough, shortness of breath, high fever, muscle pains, and headaches.[2] Nausea, vomiting, and diarrhea may also occur.[1] This often begins 2–10 days after exposure.[2]
The bacterium is found naturally in fresh water.[4] It can contaminate hot water tanks, hot tubs, and cooling towers of large air conditioners.[4] It is usually spread by breathing in mist that contains the bacteria.[4] It can also occur when contaminated water is aspirated.[4]
"""
pneumonia caused by contaminated hot water tanks
(for this reason, you need to be careful with hot water installations in unused houses)
https://en.wikipedia.org/wiki/Legionnaires%27_disease
"""
Legionnaires' disease, also known as legionellosis, is a form of atypical pneumonia caused by any type of Legionella bacteria.[3] Signs and symptoms include cough, shortness of breath, high fever, muscle pains, and headaches.[2] Nausea, vomiting, and diarrhea may also occur.[1] This often begins 2–10 days after exposure.[2]
The bacterium is found naturally in fresh water.[4] It can contaminate hot water tanks, hot tubs, and cooling towers of large air conditioners.[4] It is usually spread by breathing in mist that contains the bacteria.[4] It can also occur when contaminated water is aspirated.[4]
"""
¶Centipedes
"""
Centipedes can inflict painful stings, but most are small and rarely sting humans. They live in damp places and hunt for prey at night. Centipedes are considered beneficial because they help control household pests such as cockroaches, silverfish, and ants.
"""
https://www.poison.org/articles/are-centipede-stings-harmful-191
https://en.wikipedia.org/wiki/Centipede_bite
https://www.orkin.com/other/centipedes/centipede-bite
"""
Centipedes can inflict painful stings, but most are small and rarely sting humans. They live in damp places and hunt for prey at night. Centipedes are considered beneficial because they help control household pests such as cockroaches, silverfish, and ants.
"""
https://www.poison.org/articles/are-centipede-stings-harmful-191
https://en.wikipedia.org/wiki/Centipede_bite
https://www.orkin.com/other/centipedes/centipede-bite
¶Psocoptera / "psocids / "book lice"
* nymphs (~1mm) can be mistaken for bed bugs, or termites
* they do not bite, are not considered a problem
"""
Psocids have chewing mouthparts, but they do not bite people or pets. When they invade kitchens, they can contaminate open packages of food.
"""
______________
"""The species known as booklice received their common name because they are commonly found amongst old books—they feed upon the paste used in binding. The barklice are found on trees, feeding on algae and lichen. No member of this order is currently considered endangered; in fact, in 2007, Atlantopsocus adustus, a species native to Madeira and the Canary Islands, was found to have colonized the mild Cornish coast of southwest England."""
to be found @Fuerte ... and maybe eating on Trucko :D
log: found summer of 2020
https://www.researchgate.net/publication/230855219_The_genus_Atlantopsocus_Badonnel_Psocoptera_Psocidae_in_the_Iberian_Peninsula
https://www.researchgate.net/publication/230854979_Revision_of_the_Cerobasis_annulata_group_Psocoptera_Trogiidae_from_the_Canary_Islands
* nymphs (~1mm) can be mistaken for bed bugs, or termites
* they do not bite, are not considered a problem
"""
Psocids have chewing mouthparts, but they do not bite people or pets. When they invade kitchens, they can contaminate open packages of food.
"""
______________
"""The species known as booklice received their common name because they are commonly found amongst old books—they feed upon the paste used in binding. The barklice are found on trees, feeding on algae and lichen. No member of this order is currently considered endangered; in fact, in 2007, Atlantopsocus adustus, a species native to Madeira and the Canary Islands, was found to have colonized the mild Cornish coast of southwest England."""
to be found @Fuerte ... and maybe eating on Trucko :D
log: found summer of 2020
https://www.researchgate.net/publication/230855219_The_genus_Atlantopsocus_Badonnel_Psocoptera_Psocidae_in_the_Iberian_Peninsula
https://www.researchgate.net/publication/230854979_Revision_of_the_Cerobasis_annulata_group_Psocoptera_Trogiidae_from_the_Canary_Islands
¶Pubic lice / "crabs" (Pthirus pubis) → Pediculosis pubis
https://en.wikipedia.org/wiki/Pediculosis_pubis
* quite big, can be spotted with naked eye (~1-2mm)
* pubic regions & eyelashes
https://en.wikipedia.org/wiki/Pediculosis_pubis
* quite big, can be spotted with naked eye (~1-2mm)
* pubic regions & eyelashes
¶Common carpet beetle → rash
https://www.healthline.com/health/do-carpet-beetles-bite
"""
Carpet beetle rash
Some people can be allergic to carpet beetles, although most aren’t. Specifically, the allergy is to larvae bristles or skin that’s been shed.
They can cause an allergic reaction if they come into contact with your:
[...]
In general, they only eat natural, animal-based fabrics such as:
https://www.healthline.com/health/do-carpet-beetles-bite
"""
Carpet beetle rash
Some people can be allergic to carpet beetles, although most aren’t. Specifically, the allergy is to larvae bristles or skin that’s been shed.
They can cause an allergic reaction if they come into contact with your:
- skin
- eyes
- airways
- digestive tract
- red, itchy, and watery eyes
- runny nose
- itchy skin
- rash, which looks like welts or bites, and may cause a burning sensation
- hives
- gastrointestinal issues
[...]
In general, they only eat natural, animal-based fabrics such as:
- wool
- feathers
- felt
- fur
- silk
- leather
¶"SUPERBUGS" (antibiotic-resistant bacteria)
https://www.everydayhealth.com/infectious-diseases/superbugs-kill-a-person-every-minutes-in-us/
"""
Superbugs Kill a Person Every 15 Minutes in the United States
A new CDC report lists 18 antibiotic-resistant germs, adding two more to its 'urgent' list.
[...]
Carbapenem-resistant Acinetobacter is the kind of bacteria that’s really driving antibiotic resistance around the world, according to Fabre.
[...]
The three other urgent threats on the CDC list are:
https://en.wikipedia.org/wiki/Clostridioides_difficile_infection
"""
Clostridioides difficile infection[5] (CDI or C-diff), also known as Clostridium difficile infection, is a symptomatic infection due to the spore-forming bacterium Clostridioides difficile.[2][6] Symptoms include watery diarrhea, fever, nausea, and abdominal pain.[1] It makes up about 20% of cases of antibiotic-associated diarrhea.[1] Antibiotics can contribute to detrimental changes in gut microbiota; specifically, they decrease short-chain fatty acid absorption which results in osmotic, or watery, diarrhea.[7] Complications may include pseudomembranous colitis, toxic megacolon, perforation of the colon, and sepsis.[1]
"""
as of 2020/08 ...
https://www.cdc.gov/drugresistance/biggest-threats.html
"""
Urgent Threats
——————
https://en.wikipedia.org/wiki/Antibiotic_sensitivity_testing
https://www.everydayhealth.com/infectious-diseases/superbugs-kill-a-person-every-minutes-in-us/
"""
Superbugs Kill a Person Every 15 Minutes in the United States
A new CDC report lists 18 antibiotic-resistant germs, adding two more to its 'urgent' list.
[...]
Carbapenem-resistant Acinetobacter is the kind of bacteria that’s really driving antibiotic resistance around the world, according to Fabre.
[...]
The three other urgent threats on the CDC list are:
- Clostridioides difficile (C. diff), a bacteria that can cause life-threatening diarrhea and colitis (inflammation of the colon)
- Carbapenem-resistant Enterobacteriaceae, also known as "nightmare bacteria," which are resistant to nearly all antibiotics
- Drug-resistant Neisseria gonorrhoeae, which causes the sexually transmitted disease gonorrhea.
https://en.wikipedia.org/wiki/Clostridioides_difficile_infection
"""
Clostridioides difficile infection[5] (CDI or C-diff), also known as Clostridium difficile infection, is a symptomatic infection due to the spore-forming bacterium Clostridioides difficile.[2][6] Symptoms include watery diarrhea, fever, nausea, and abdominal pain.[1] It makes up about 20% of cases of antibiotic-associated diarrhea.[1] Antibiotics can contribute to detrimental changes in gut microbiota; specifically, they decrease short-chain fatty acid absorption which results in osmotic, or watery, diarrhea.[7] Complications may include pseudomembranous colitis, toxic megacolon, perforation of the colon, and sepsis.[1]
"""
as of 2020/08 ...
https://www.cdc.gov/drugresistance/biggest-threats.html
"""
Urgent Threats
- Carbapenem-resistant Acinetobacter
- Candida auris
- Clostridioides difficile
- Carbapenem-resistant Enterobacteriaceae
- Drug-resistant Neisseria gonorrhoeae
- Drug-resistant Campylobacter
- Drug-resistant Candida
- ESBL-producing Enterobacteriaceae
- Vancomycin-resistant Enterococci (VRE)
- Multidrug-resistant Pseudomonas aeruginosa
- Drug-resistant nontyphoidal Salmonella
- Drug-resistant Salmonella serotype Typhi
- Drug-resistant Shigella
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Drug-resistant Streptococcus pneumoniae
- Drug-resistant Tuberculosis
- Erythromycin-Resistant Group A Streptococcus
- Clindamycin-resistant Group B Streptococcus
- Azole-resistant Aspergillus fumigatus
- Drug-resistant Mycoplasma genitalium
- Drug-resistant Bordetella pertussis
——————
https://en.wikipedia.org/wiki/Antibiotic_sensitivity_testing
¶[M??] Weird small (3mm) biting fly in fuerte ... "black fly"?
[!!]
not a biting midge, more like a reduced size normal fly
known all 2020
typical behaviour:
super fast
circles around you, then dissapears
you smash it and it's always destroyed
every time i see it, i get itchy bites on lower scalp and around ears
[!!]
not a biting midge, more like a reduced size normal fly
known all 2020
typical behaviour:
super fast
circles around you, then dissapears
you smash it and it's always destroyed
every time i see it, i get itchy bites on lower scalp and around ears
¶FUNGAL— candida → jock itch
"""
Infections caused by fungus and yeasts: Candida (yeast), Trichophyton, and Epidermophyton (fungal molds)
Jock itch is most common in older, obese adults and athletes.
"""
[!!] learn to recognize & separate
#diagnostics
"""
Infections caused by fungus and yeasts: Candida (yeast), Trichophyton, and Epidermophyton (fungal molds)
Jock itch is most common in older, obese adults and athletes.
"""
[!!] learn to recognize & separate
#diagnostics
¶Clover mites
https://en.wikipedia.org/wiki/Bryobia_praetiosa
NOT HARMFUL
Clover mites are not harmful to humans, pets, or furniture.[4]
https://en.wikipedia.org/wiki/Bryobia_praetiosa
NOT HARMFUL
Clover mites are not harmful to humans, pets, or furniture.[4]
¶"Springtails" / springtail mites
https://www.orkin.com/other/springtails
"Size: Springtails are tiny insects. Their size ranges from 0.25 to 6 mm."
Kind of like fleas.
NOT BITING
"""
Springtails are just a nuisance; they do not cause damage or harm. However, if the pests find an appropriate breeding place inside, they will gather in large numbers and this may cause immense frustration and stress for residents
"""
https://www.orkin.com/other/springtails
"Size: Springtails are tiny insects. Their size ranges from 0.25 to 6 mm."
Kind of like fleas.
NOT BITING
"""
Springtails are just a nuisance; they do not cause damage or harm. However, if the pests find an appropriate breeding place inside, they will gather in large numbers and this may cause immense frustration and stress for residents
"""
¶@sea: Seabather's eruption
aka "Sea lice" (but misnomer, as this is a fish-only parasite)
esp: Erupción del bañista
https://en.wikipedia.org/wiki/Thimble_jellyfish#Seabather's_eruption
https://www.cigna.com/individuals-families/health-wellness/hw-en-espanol/temas-de-salud/erupcion-del-banista-tm6356spec
"""
This type of rash can also be a symptom of Sea bather's eruption. This stinging, pruritic, maculopapular rash affects swimmers in some Atlantic locales (e.g., Florida, Caribbean, Long Island). It is caused by hypersensitivity to stings from the larvae of the sea anemone (e.g., Edwardsiella lineate) or the thimble jellyfish (Linuche unguiculata). The rash appears where the bathing suit contacts the skin.[5]
"""
https://en.wikipedia.org/wiki/Maculopapular_rash
After contact
http://www.buysafesea.com/sea_lice.php
"""
If you suspect you've been exposed to sea lice, exit the water immediately, remove your bathing suit, and shower thoroughly. Do not rinse with fresh water while still wearing the suit as this will cause the stinging cells still in the fabric to fire, releasing even more venom. Do not wear the same swimsuit again until it's been thoroughly machine washed and dried
"""
____________________________________
In Canaries: ???
aka "Sea lice" (but misnomer, as this is a fish-only parasite)
esp: Erupción del bañista
https://en.wikipedia.org/wiki/Thimble_jellyfish#Seabather's_eruption
https://www.cigna.com/individuals-families/health-wellness/hw-en-espanol/temas-de-salud/erupcion-del-banista-tm6356spec
"""
This type of rash can also be a symptom of Sea bather's eruption. This stinging, pruritic, maculopapular rash affects swimmers in some Atlantic locales (e.g., Florida, Caribbean, Long Island). It is caused by hypersensitivity to stings from the larvae of the sea anemone (e.g., Edwardsiella lineate) or the thimble jellyfish (Linuche unguiculata). The rash appears where the bathing suit contacts the skin.[5]
"""
https://en.wikipedia.org/wiki/Maculopapular_rash
After contact
http://www.buysafesea.com/sea_lice.php
"""
If you suspect you've been exposed to sea lice, exit the water immediately, remove your bathing suit, and shower thoroughly. Do not rinse with fresh water while still wearing the suit as this will cause the stinging cells still in the fabric to fire, releasing even more venom. Do not wear the same swimsuit again until it's been thoroughly machine washed and dried
"""
____________________________________
In Canaries: ???
¶@sea: "Sea sawdust" (Trichodesmium erythraeum)
In Canary islands:
https://www.lanzaroteguidebook.com/news/news/details-1750/toxic-tales-come-on-in-the-water%C2%B4s-lovely
"""
the Canary Islands Government, via Health Minister José Manuel Baltar, has clarified that health and environmental experts guarantee that the presence of microalgal blooms at a small number of Canary Islands beaches is a sporadic and natural event caused by a rare combination of biological, environmental and climatological factors.
"""
"""
The only effect of microalgae is skin irritation and the Canary Islands Health Authorities therefore recommend that people avoid direct skin contact with the blooms. These are easy to identify due to their characteristic appearance and colour. It must be noted that the Canary Islands Public Health System has not seen any variation in the number of reported cases of skin irritation since the start of the phenomenon."
[...]
The algae are a type of bacteria, trichodesmium erythraeum, also known as sea sawdust, said Aleman.
The bacterium "contains a toxin which can lead to skin irritation, dermatitis, hence one must avoid coming into contact with it in the water and on the sand."
"""
https://phys.org/news/2017-08-algae-blooms-irk-canaries-beachgoers.html
https://en.wikipedia.org/wiki/Trichodesmium_erythraeum
________________
https://news.sky.com/story/tourists-warned-to-avoid-toxic-sea-sawdust-microalgae-off-canary-islands-10978940
https://www.theguardian.com/world/2017/aug/08/canary-island-tourists-warned-to-avoid-toxic-sea-sawdust-algae
blooms specific to conditions
"""
Marta Sanson, professor of plant biology at Tenerife’s La Laguna university, said that “ideal conditions are allowing proliferation of these micro-algae”.
Those include “an increase in water temperature” as well as a “dust cloud sweeping in off the Sahara which is rich in iron, a nutrient which micro-organisms like”.
"""
In Canary islands:
https://www.lanzaroteguidebook.com/news/news/details-1750/toxic-tales-come-on-in-the-water%C2%B4s-lovely
"""
the Canary Islands Government, via Health Minister José Manuel Baltar, has clarified that health and environmental experts guarantee that the presence of microalgal blooms at a small number of Canary Islands beaches is a sporadic and natural event caused by a rare combination of biological, environmental and climatological factors.
"""
"""
The only effect of microalgae is skin irritation and the Canary Islands Health Authorities therefore recommend that people avoid direct skin contact with the blooms. These are easy to identify due to their characteristic appearance and colour. It must be noted that the Canary Islands Public Health System has not seen any variation in the number of reported cases of skin irritation since the start of the phenomenon."
[...]
The algae are a type of bacteria, trichodesmium erythraeum, also known as sea sawdust, said Aleman.
The bacterium "contains a toxin which can lead to skin irritation, dermatitis, hence one must avoid coming into contact with it in the water and on the sand."
"""
https://phys.org/news/2017-08-algae-blooms-irk-canaries-beachgoers.html
https://en.wikipedia.org/wiki/Trichodesmium_erythraeum
________________
https://news.sky.com/story/tourists-warned-to-avoid-toxic-sea-sawdust-microalgae-off-canary-islands-10978940
https://www.theguardian.com/world/2017/aug/08/canary-island-tourists-warned-to-avoid-toxic-sea-sawdust-algae
blooms specific to conditions
"""
Marta Sanson, professor of plant biology at Tenerife’s La Laguna university, said that “ideal conditions are allowing proliferation of these micro-algae”.
Those include “an increase in water temperature” as well as a “dust cloud sweeping in off the Sahara which is rich in iron, a nutrient which micro-organisms like”.
"""
¶_____ NEW / UNSORTED _____
¶TICKS— Lone star ticks / red mites? → Alpha-gal syndrome
"""
Alpha-gal syndrome is a recently identified type of food allergy to red meat. In the United States, the condition most often begins when a Lone Star tick bite transmits a sugar molecule called alpha-gal into the body.Jul 13, 2019
[...]
Researchers now believe that some people who have frequent, unexplained anaphylactic reactions — and who test negative for other food allergies — may be affected by alpha-gal syndrome. There's no treatment other than avoiding red meat.
"""
https://www.mayoclinic.org/diseases-conditions/alpha-gal-syndrome/symptoms-causes/syc-20428608
https://www.technologynetworks.com/applied-sciences/news/meat-allergy-spread-limited-by-fire-ants-but-at-a-price-336635
"""
Alpha-gal syndrome is a recently identified type of food allergy to red meat. In the United States, the condition most often begins when a Lone Star tick bite transmits a sugar molecule called alpha-gal into the body.Jul 13, 2019
[...]
Researchers now believe that some people who have frequent, unexplained anaphylactic reactions — and who test negative for other food allergies — may be affected by alpha-gal syndrome. There's no treatment other than avoiding red meat.
"""
https://www.mayoclinic.org/diseases-conditions/alpha-gal-syndrome/symptoms-causes/syc-20428608
https://www.technologynetworks.com/applied-sciences/news/meat-allergy-spread-limited-by-fire-ants-but-at-a-price-336635
¶(Water-contact + mammals→) Leptospirosis
... including rodents, cats, sheep, etc.
https://en.wikipedia.org/wiki/Leptospirosis
q: how does an infected animal, for example, feral cat look like?
human symptoms: jaundice + conjunctivitis
... including rodents, cats, sheep, etc.
https://en.wikipedia.org/wiki/Leptospirosis
q: how does an infected animal, for example, feral cat look like?
human symptoms: jaundice + conjunctivitis
¶(Rodents→) Hantavirus
ESP: "La fiebre hemorrágica con síndrome renal (FHSR, HFRS por sus siglas en inglés) es un grupo de enfermedades clínicamente similares causadas por especies de hantavirus de la familia Hantaviridae"
https://www.mayoclinic.org/diseases-conditions/hantavirus-pulmonary-syndrome/symptoms-causes/syc-20351838
"""
Hantavirus pulmonary syndrome is an infectious disease characterized by flu-like symptoms that can progress rapidly to potentially life-threatening breathing problems.
[...]
If you've been around rodents or rodent droppings and have signs and symptoms of fever, chills, muscle aches or any difficulties breathing, seek immediate medical attention.
"""
https://en.wikipedia.org/wiki/Hantavirus_hemorrhagic_fever_with_renal_syndrome
Causes Hantavirus hemorrhagic fever with renal syndrome
"""
The species that cause HFRS include Hantaan orthohantavirus, Dobrava-Belgrade orthohantavirus, Saaremaa virus, Seoul orthohantavirus, Puumala orthohantavirus and other orthohantaviruses. It is found in Europe, Asia, and Africa.[1] Of these species, Hantaan River virus and Dobrava-Belgrade virus cause the most severe form of the syndrome and have the highest morbidity rates. When caused by the Puumala virus, it is also called nephropathia epidemica.
"""
Late to show symptoms:
"Symptoms of HFRS usually develop within 1 to 2 weeks after exposure to infectious material, but in rare cases, they may take up to 8 weeks to develop."
_________
(SLO)
There was a 2021 outbreak in Slovenia.
https://www.nijz.si/sl/tedensko-spremljanje-hemoragicne-mrzlice-z-renalnim-sindromom-hmrs
(good report & advice!)
https://sl.wikipedia.org/wiki/Virus_Dobrava
https://sl.wikipedia.org/wiki/Mi%C5%A1ja_mrzlica
ESP: "La fiebre hemorrágica con síndrome renal (FHSR, HFRS por sus siglas en inglés) es un grupo de enfermedades clínicamente similares causadas por especies de hantavirus de la familia Hantaviridae"
https://www.mayoclinic.org/diseases-conditions/hantavirus-pulmonary-syndrome/symptoms-causes/syc-20351838
"""
Hantavirus pulmonary syndrome is an infectious disease characterized by flu-like symptoms that can progress rapidly to potentially life-threatening breathing problems.
[...]
If you've been around rodents or rodent droppings and have signs and symptoms of fever, chills, muscle aches or any difficulties breathing, seek immediate medical attention.
"""
https://en.wikipedia.org/wiki/Hantavirus_hemorrhagic_fever_with_renal_syndrome
Causes Hantavirus hemorrhagic fever with renal syndrome
"""
The species that cause HFRS include Hantaan orthohantavirus, Dobrava-Belgrade orthohantavirus, Saaremaa virus, Seoul orthohantavirus, Puumala orthohantavirus and other orthohantaviruses. It is found in Europe, Asia, and Africa.[1] Of these species, Hantaan River virus and Dobrava-Belgrade virus cause the most severe form of the syndrome and have the highest morbidity rates. When caused by the Puumala virus, it is also called nephropathia epidemica.
"""
Late to show symptoms:
"Symptoms of HFRS usually develop within 1 to 2 weeks after exposure to infectious material, but in rare cases, they may take up to 8 weeks to develop."
_________
(SLO)
There was a 2021 outbreak in Slovenia.
https://www.nijz.si/sl/tedensko-spremljanje-hemoragicne-mrzlice-z-renalnim-sindromom-hmrs
(good report & advice!)
¶ Cleaning up after rodents (rats)
"""
Safe cleanup procedures
Wet down dead rodents and areas where rodents have been with alcohol, household disinfectants or bleach.
This kills the virus and helps prevent infected dust from being stirred up into the air. Once everything is wet, use a damp towel to pick up the contaminated material.
Then mop or sponge the area with disinfectant.
"""
"""
Safe cleanup procedures
Wet down dead rodents and areas where rodents have been with alcohol, household disinfectants or bleach.
This kills the virus and helps prevent infected dust from being stirred up into the air. Once everything is wet, use a damp towel to pick up the contaminated material.
Then mop or sponge the area with disinfectant.
"""
¶COVID-19
aka coronavirus
aka SARS-CoV-19
The 2020 pandemic.
→ 🔗pandemic
-------------------------------------------
"""
Nirmatrelvir, ritonavir, remdesivir and molnupiravir are antiviral medicines. Sotrovimab is a biological medicine also known as a neutralising monoclonal antibody (nMAb). Sotrovimab may be given to people if antiviral medicines are unsuitable for them to take.
"""
aka coronavirus
aka SARS-CoV-19
The 2020 pandemic.
→ 🔗pandemic
-------------------------------------------
"""
Nirmatrelvir, ritonavir, remdesivir and molnupiravir are antiviral medicines. Sotrovimab is a biological medicine also known as a neutralising monoclonal antibody (nMAb). Sotrovimab may be given to people if antiviral medicines are unsuitable for them to take.
"""
¶Staphylococcus aureus
https://www.mayoclinic.org/diseases-conditions/staph-infections/symptoms-causes/syc-20356221
"""
Overview
Staph infections are caused by staphylococcus bacteria, types of germs commonly found on the skin or in the nose of even healthy individuals. Most of the time, these bacteria cause no problems or result in relatively minor skin infections.
But staph infections can turn deadly if the bacteria invade deeper into your body, entering your bloodstream, joints, bones, lungs or heart. A growing number of otherwise healthy people are developing life-threatening staph infections.
Treatment usually involves antibiotics and drainage of the infected area. However, some staph infections no longer respond to common antibiotics.
-------
Symptoms
Staph infections can range from minor skin problems to endocarditis, a life-threatening infection of the inner lining of your heart (endocardium). Because of this, signs and symptoms of staph infections vary widely, depending on the location and severity of the infection.
Skin infections caused by staph bacteria include:
"""
Food poisoning:
Staph bacteria are one of the most common causes of food poisoning.
Symptoms come on quickly, usually within hours of eating a contaminated food.
Symptoms usually disappear quickly, too, often lasting just half a day.
"""
Tranmisssion
"These bacteria can also be transmitted from person to person. Because staph bacteria are so hardy, they can live on objects such as pillowcases or towels long enough to transfer to the next person who touches them."
Prevention
"""
#laundry
__________________
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942668/
Staphylococcus aureus toxins
"""
Staphylococcus aureus is a dangerous and versatile pathogen that can cause a multitude of different diseases. Most frequently, it causes skin infections and infections of the respiratory tract. Skin infections are usually community-acquired, whereas infections of the lung dominate among nosocomial S. aureus infections. Among nosocomial pathogens, S. aureus is the most common and associated with high morbidity and mortality. S. aureus pneumonia often develops in hospitalized patients with underlying conditions, such as in patients suffering from immune deficiencies or viral infections. However, S. aureus may also cause a variety of other sometimes very severe and life-threatening diseases, such as infective endocarditis, toxic shock syndrome, scalded skin syndrome, or osteomyelitis, to name but a few. Even necrotizing fasciitis and necrotizing pneumonia were reported with S. aureus as the causative agent
"""
https://www.mayoclinic.org/diseases-conditions/staph-infections/symptoms-causes/syc-20356221
"""
Overview
Staph infections are caused by staphylococcus bacteria, types of germs commonly found on the skin or in the nose of even healthy individuals. Most of the time, these bacteria cause no problems or result in relatively minor skin infections.
But staph infections can turn deadly if the bacteria invade deeper into your body, entering your bloodstream, joints, bones, lungs or heart. A growing number of otherwise healthy people are developing life-threatening staph infections.
Treatment usually involves antibiotics and drainage of the infected area. However, some staph infections no longer respond to common antibiotics.
-------
Symptoms
Staph infections can range from minor skin problems to endocarditis, a life-threatening infection of the inner lining of your heart (endocardium). Because of this, signs and symptoms of staph infections vary widely, depending on the location and severity of the infection.
Skin infections caused by staph bacteria include:
- Boils. The most common type of staph infection is the boil, a pocket of pus that develops in a hair follicle or oil gland. The skin over the infected area usually becomes red and swollen.
- If a boil breaks open, it will probably drain pus. Boils occur most often under the arms or around the groin or buttocks.
- Impetigo. This contagious, often painful rash can be caused by staph bacteria. Impetigo usually features large blisters that may ooze fluid and develop a honey-colored crust.
- Cellulitis. Cellulitis — an infection of the deeper layers of skin — causes skin redness and swelling on the surface of your skin. Sores or areas of oozing discharge may develop, too.
- Staphylococcal scalded skin syndrome. Toxins produced as a result of a staph infection may lead to staphylococcal scalded skin syndrome. Affecting mostly babies and children, this condition features a fever, a rash and sometimes blisters. When the blisters break, the top layer of skin comes off — leaving a red, raw surface that looks like a burn.
"""
Food poisoning:
Staph bacteria are one of the most common causes of food poisoning.
Symptoms come on quickly, usually within hours of eating a contaminated food.
Symptoms usually disappear quickly, too, often lasting just half a day.
"""
Tranmisssion
"These bacteria can also be transmitted from person to person. Because staph bacteria are so hardy, they can live on objects such as pillowcases or towels long enough to transfer to the next person who touches them."
Prevention
"""
- Wash clothing and bedding in hot water. Staph bacteria can survive on clothing and bedding that isn't properly washed. To get bacteria off clothing and sheets, wash them in hot water whenever possible.
- Also, use bleach on any bleach-safe materials. Drying in the dryer is better than air-drying, but staph bacteria may survive the clothes dryer.
#laundry
__________________
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942668/
Staphylococcus aureus toxins
"""
Staphylococcus aureus is a dangerous and versatile pathogen that can cause a multitude of different diseases. Most frequently, it causes skin infections and infections of the respiratory tract. Skin infections are usually community-acquired, whereas infections of the lung dominate among nosocomial S. aureus infections. Among nosocomial pathogens, S. aureus is the most common and associated with high morbidity and mortality. S. aureus pneumonia often develops in hospitalized patients with underlying conditions, such as in patients suffering from immune deficiencies or viral infections. However, S. aureus may also cause a variety of other sometimes very severe and life-threatening diseases, such as infective endocarditis, toxic shock syndrome, scalded skin syndrome, or osteomyelitis, to name but a few. Even necrotizing fasciitis and necrotizing pneumonia were reported with S. aureus as the causative agent
"""
¶CA-MRSA (resistant Staph)
https://www.cedars-sinai.org/health-library/diseases-and-conditions/c/community-acquired-mrsa.html
"""
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of bacteria. Unlike other Staph bacteria, it can’t be killed by the antibiotic methicillin and other similar medicines and is therefore called methicillin-resistant. Community-acquired means that you didn’t get the infection in a hospital or other healthcare setting. MRSA infections are sometimes very hard to treat.
"""
https://www.healthline.com/health/mrsa?utm_source=ReadNext
"""
Methicillin-resistant Staphylococcus aureus (MRSA) is an infection of Staphylococcus (staph) bacteria. Staph infections can cause bumps, sores, and blisters on the skin. In severe cases, they can cause blood poisoning and shock.
"""
via hospital
"""
HA-MRSA is generally more likely to cause serious complications, such as pneumonia, urinary tract infections (UTIs), and the blood infection sepsis. It’s important to see your doctor right away if you notice any of the following symptoms:
via community
"""
Symptoms of CA-MRSA
CA-MRSA usually causes skin infections. Areas that have increased body hair, such as the armpits or back of the neck, are more likely to be infected.
Areas that have been cut, scratched, or rubbed are also vulnerable to infection because your biggest barrier to germs — your skin — has been damaged.
The infection usually causes a swollen, painful bump to form on the skin. The bump may resemble a spider bite or pimple. It often has a yellow or white center and a central head.
Sometimes an infected area is surrounded by an area of redness and warmth, known as cellulitis. Pus and other fluids may drain from the affected area. Some people also experience a fever.
"""
PREVENTION
"""
How can MRSA be prevented?
Take the following measures to reduce your risk of getting and spreading CA-MRSA:
[!!!→] #manual
https://www.cedars-sinai.org/health-library/diseases-and-conditions/c/community-acquired-mrsa.html
"""
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of bacteria. Unlike other Staph bacteria, it can’t be killed by the antibiotic methicillin and other similar medicines and is therefore called methicillin-resistant. Community-acquired means that you didn’t get the infection in a hospital or other healthcare setting. MRSA infections are sometimes very hard to treat.
"""
https://www.healthline.com/health/mrsa?utm_source=ReadNext
"""
Methicillin-resistant Staphylococcus aureus (MRSA) is an infection of Staphylococcus (staph) bacteria. Staph infections can cause bumps, sores, and blisters on the skin. In severe cases, they can cause blood poisoning and shock.
"""
via hospital
"""
HA-MRSA is generally more likely to cause serious complications, such as pneumonia, urinary tract infections (UTIs), and the blood infection sepsis. It’s important to see your doctor right away if you notice any of the following symptoms:
- rash
- headaches
- muscle aches
- chills
- fever
- fatigue
- cough
- shortness of breath
- chest pain
via community
"""
Symptoms of CA-MRSA
CA-MRSA usually causes skin infections. Areas that have increased body hair, such as the armpits or back of the neck, are more likely to be infected.
Areas that have been cut, scratched, or rubbed are also vulnerable to infection because your biggest barrier to germs — your skin — has been damaged.
The infection usually causes a swollen, painful bump to form on the skin. The bump may resemble a spider bite or pimple. It often has a yellow or white center and a central head.
Sometimes an infected area is surrounded by an area of redness and warmth, known as cellulitis. Pus and other fluids may drain from the affected area. Some people also experience a fever.
"""
PREVENTION
"""
How can MRSA be prevented?
Take the following measures to reduce your risk of getting and spreading CA-MRSA:
- Wash your hands on a regular basis. This is the first line of defense against spreading MRSA. Scrub your hands for at least 15 seconds before drying them with a towel. Use another towel to turn off the faucet. Carry hand sanitizer that contains 60 percent alcohol. Use it to keep your hands clean when you don’t have access to soap and water.
- Keep your wounds covered at all times. Covering wounds can prevent pus or other fluids containing staph bacteria from contaminating surfaces that other people may touch.
- Don’t share personal items. This includes towels, sheets, razors, and athletic equipment.
- Sanitize your linens. If you have cuts or broken skin, wash bed linens and towels in hot water with extra bleach and dry everything at high heat in the dryer. You should also wash your gym and athletic clothes after each use.
[!!!→] #manual
¶(blackflies→) Onchocerca volvulus worms → Onchocerciasis ("river blindness")
"""
The origins of ivermectin as a human drug are inextricably linked with Onchocerciasis (or River Blindness), a chronic human filarial disease caused by infection with Onchocerca volvulus worms. The parasites are transmitted via the bite of infected blackflies of the genus Simulium, which breed in highly-oxygenated, fast-flowing rivers and watercourses. In the human body, immature larval forms of the parasite create nodules in subcutaneous tissue, where they mature into adult worms. After mating, female worms can release up to 1000 microfilariae a day for some 10–14 years. These move through the body, and when they die they cause a variety of conditions, including skin rashes, lesions, intense itching, oedema and skin depigmentation (Fig. (Fig.2 ).2 ). Microfilariae also invade the eye, causing visual impairment and loss of vision, onchocerciasis being the second leading cause of blindness caused by an infectious disease.17) The disease causes visual damage for some 1–2 million people, around half of who will become blind.18)
"""
"""
The origins of ivermectin as a human drug are inextricably linked with Onchocerciasis (or River Blindness), a chronic human filarial disease caused by infection with Onchocerca volvulus worms. The parasites are transmitted via the bite of infected blackflies of the genus Simulium, which breed in highly-oxygenated, fast-flowing rivers and watercourses. In the human body, immature larval forms of the parasite create nodules in subcutaneous tissue, where they mature into adult worms. After mating, female worms can release up to 1000 microfilariae a day for some 10–14 years. These move through the body, and when they die they cause a variety of conditions, including skin rashes, lesions, intense itching, oedema and skin depigmentation (Fig. (Fig.2 ).2 ). Microfilariae also invade the eye, causing visual impairment and loss of vision, onchocerciasis being the second leading cause of blindness caused by an infectious disease.17) The disease causes visual damage for some 1–2 million people, around half of who will become blind.18)
"""
¶Silverfish
https://en.wikipedia.org/wiki/Silverfish
"""
The silverfish is an agile runner and can outrun most of its predators (including wandering spiders and centipedes). However, such running is possible only on horizontal surfaces, as it lacks any additional appendages, and therefore is not fast enough to climb walls at the same speed.[citation needed] It also avoids light.[10]
They inhabit moist areas, requiring a relative humidity between 75% and 95%.
Silverfish are able to digest cellulose by themselves, thanks to the cellulase that is produced by its midgut.[9] They consume matter that contains polysaccharides, such as starches and dextrin in adhesives.[4] These include book bindings, carpet, clothing, coffee, dandruff, glue, hair, some paints, paper, photos, plaster, and sugar. They will damage wallpaper in order to consume the paste.[17] Silverfish can also cause damage to tapestries. Other substances they may eat include cotton, dead insects, linen, silk, leftover crumbs, or even their own exuviae (moulted exoskeleton). During famine, a silverfish may even consume leatherware and synthetic fabrics. Silverfish can live for a year or more without eating if water is available
Silverfish are considered household pests, due to their consumption and destruction of property.[2]
However, although they are responsible for the contamination of food and other types of damage, they do not transmit disease.[4][19] Earwigs, house centipedes, and spiders such as the spitting spider Scytodes thoracica are known to be predators of silverfish.
Together with jumping bristletails, the predecessors of silverfish are considered the earliest, most primitive insects. They evolved at the latest in mid-Devonian and possibly as early as late Silurian more than 400 million years ago
"""
https://en.wikipedia.org/wiki/Silverfish
"""
The silverfish is an agile runner and can outrun most of its predators (including wandering spiders and centipedes). However, such running is possible only on horizontal surfaces, as it lacks any additional appendages, and therefore is not fast enough to climb walls at the same speed.[citation needed] It also avoids light.[10]
They inhabit moist areas, requiring a relative humidity between 75% and 95%.
Silverfish are able to digest cellulose by themselves, thanks to the cellulase that is produced by its midgut.[9] They consume matter that contains polysaccharides, such as starches and dextrin in adhesives.[4] These include book bindings, carpet, clothing, coffee, dandruff, glue, hair, some paints, paper, photos, plaster, and sugar. They will damage wallpaper in order to consume the paste.[17] Silverfish can also cause damage to tapestries. Other substances they may eat include cotton, dead insects, linen, silk, leftover crumbs, or even their own exuviae (moulted exoskeleton). During famine, a silverfish may even consume leatherware and synthetic fabrics. Silverfish can live for a year or more without eating if water is available
Silverfish are considered household pests, due to their consumption and destruction of property.[2]
However, although they are responsible for the contamination of food and other types of damage, they do not transmit disease.[4][19] Earwigs, house centipedes, and spiders such as the spitting spider Scytodes thoracica are known to be predators of silverfish.
Together with jumping bristletails, the predecessors of silverfish are considered the earliest, most primitive insects. They evolved at the latest in mid-Devonian and possibly as early as late Silurian more than 400 million years ago
"""
¶Campylobacter jejuni (→ food poisoning)
https://en.wikipedia.org/wiki/Campylobacter_jejuni
"Campylobacter jejuni (/ˈkæmpɪloʊˌbæktər dʒəˈdʒuːni/) is one of the most common causes of food poisoning ... The European Food Safety Authority reported 246,571 cases in 2018, and estimated approximately nine million cases of human campylobacteriosis per year in the European Union.[3]
Campylobacter jejuni is in a genus of bacteria that is among the most common causes of bacterial infections in humans worldwide.
C. jejuni is commonly associated with poultry, and is also commonly found in animal feces.
It has been linked with subsequent development of Guillain–Barré syndrome, which usually develops two to three weeks after the initial illness.[12] Individuals with recent C. jejuni infections develop Guillain-Barré syndrome at a rate of 0.3 per 1000 infections, about 100 times more often than the general population.[13] Another chronic condition that may be associated with Campylobacter infection is reactive arthritis.[14] Reactive arthritis is a complication strongly associated with a particular genetic make-up. That is, persons who have the human leukocyte antigen B27 (HLA-B27) are most susceptible. Most often, the symptoms of reactive arthritis will occur up to several weeks after infection.[4][15]
[...]
"Campylobacteriosis is an infectious disease caused by bacteria of the genus Campylobacter. In most people who become ill with campylobacteriosis, symptoms develop within two to five days of exposure to the organism and illness typically lasts seven days following onset.[2] Infection with C. jejuni usually results in enteritis, which is characterised by abdominal pain, diarrhea, fever, and malaise. Diarrhea itself can vary in severity from loose to bloody stools. The disease is usually self-limiting. However, it does respond to antibiotics
[...]
Infection results from the ingestion of contaminated food or water, and the infective dose can be as low as 800 organisms
[...]
surveys show that 20 to 100% of retail chickens are contaminated. This is not overly surprising, since many healthy chickens carry these bacteria in their intestinal tracts and often in high concentrations, up to 108 cfu/g
[...]
https://en.wikipedia.org/wiki/Campylobacter_jejuni
"Campylobacter jejuni (/ˈkæmpɪloʊˌbæktər dʒəˈdʒuːni/) is one of the most common causes of food poisoning ... The European Food Safety Authority reported 246,571 cases in 2018, and estimated approximately nine million cases of human campylobacteriosis per year in the European Union.[3]
Campylobacter jejuni is in a genus of bacteria that is among the most common causes of bacterial infections in humans worldwide.
C. jejuni is commonly associated with poultry, and is also commonly found in animal feces.
It has been linked with subsequent development of Guillain–Barré syndrome, which usually develops two to three weeks after the initial illness.[12] Individuals with recent C. jejuni infections develop Guillain-Barré syndrome at a rate of 0.3 per 1000 infections, about 100 times more often than the general population.[13] Another chronic condition that may be associated with Campylobacter infection is reactive arthritis.[14] Reactive arthritis is a complication strongly associated with a particular genetic make-up. That is, persons who have the human leukocyte antigen B27 (HLA-B27) are most susceptible. Most often, the symptoms of reactive arthritis will occur up to several weeks after infection.[4][15]
[...]
"Campylobacteriosis is an infectious disease caused by bacteria of the genus Campylobacter. In most people who become ill with campylobacteriosis, symptoms develop within two to five days of exposure to the organism and illness typically lasts seven days following onset.[2] Infection with C. jejuni usually results in enteritis, which is characterised by abdominal pain, diarrhea, fever, and malaise. Diarrhea itself can vary in severity from loose to bloody stools. The disease is usually self-limiting. However, it does respond to antibiotics
[...]
Infection results from the ingestion of contaminated food or water, and the infective dose can be as low as 800 organisms
[...]
surveys show that 20 to 100% of retail chickens are contaminated. This is not overly surprising, since many healthy chickens carry these bacteria in their intestinal tracts and often in high concentrations, up to 108 cfu/g
[...]
- Cook all poultry products thoroughly. Make sure that the meat is cooked throughout (no longer pink) and any juices run clear. All poultry should be cooked to reach a minimum internal temperature of 165 °F (74 °C).
- Prevent cross-contamination in the kitchen by using separate cutting boards for foods of animal origin and other foods and by thoroughly cleaning all cutting boards, countertops, and utensils with soap and hot water after preparing raw food of animal origin.
¶(@ANTS) ant parasite changing their social status, longevity ...
https://www.theatlantic.com/science/archive/2021/05/ant-tapeworm/618919/
https://www.theatlantic.com/science/archive/2021/05/ant-tapeworm/618919/
¶Respiratory syncytial virus
https://en.wikipedia.org/wiki/Respiratory_syncytial_virus
("also happening during Covid pandemic")
https://en.wikipedia.org/wiki/Respiratory_syncytial_virus
("also happening during Covid pandemic")
¶Black mold (Stachybotrys→mycotoxins)
https://moldpedia.com/black-mold-stachybotrys
https://swiftrestorationcompany.com/construction-honored-with-agc-best-builders/
"""
Never try to remove toxic black mold on your own. Disturbing toxic black mold can make it release huge amounts of spores and mycotoxins throughout your home, making your symptoms much worse.
"""
Jesus fucking christ
https://www.howtoremoveblackmold.com/how-to-kill-black-mold/
fucking hell ... this is a big problem
----------
Natural removal (at end):
* soda
* white vinegar
https://www.deloindom.si/enostanovanjske-hise/dom-brez-vlage-premisljeno-nad-madeze-plesen (SLO)
_______________
https://www.medicalnewstoday.com/articles/323419#_noHeaderPrefixedContent
"""
There is no single type of mold called “black mold” — many molds are black. When people use the term, they may be referring to a type called Stachybotrys chartarum (S. chartarum), also known as Stachybotrys atra.
There is no scientific evidence to suggest that exposure to S. chartarum is more dangerous than exposure to any other type of mold.
However, some people may be more sensitive to mold spores than others, and they may develop respiratory symptoms after inhaling even a small number of spores. In large quantities, mold spores can cause ill health in almost anyone.
"""
https://moldpedia.com/black-mold-stachybotrys
https://swiftrestorationcompany.com/construction-honored-with-agc-best-builders/
"""
Never try to remove toxic black mold on your own. Disturbing toxic black mold can make it release huge amounts of spores and mycotoxins throughout your home, making your symptoms much worse.
"""
Jesus fucking christ
https://www.howtoremoveblackmold.com/how-to-kill-black-mold/
fucking hell ... this is a big problem
----------
Natural removal (at end):
* soda
* white vinegar
https://www.deloindom.si/enostanovanjske-hise/dom-brez-vlage-premisljeno-nad-madeze-plesen (SLO)
_______________
https://www.medicalnewstoday.com/articles/323419#_noHeaderPrefixedContent
"""
There is no single type of mold called “black mold” — many molds are black. When people use the term, they may be referring to a type called Stachybotrys chartarum (S. chartarum), also known as Stachybotrys atra.
There is no scientific evidence to suggest that exposure to S. chartarum is more dangerous than exposure to any other type of mold.
However, some people may be more sensitive to mold spores than others, and they may develop respiratory symptoms after inhaling even a small number of spores. In large quantities, mold spores can cause ill health in almost anyone.
"""
¶ME/CFS
"""
Chronic fatigue syndrome (CFS), also called myalgic encephalomyelitis (ME) or ME/CFS, is a complex, debilitating, long-term medical condition. The causes and mechanisms of the disease are not yet fully understood. [12] Distinguishing core symptoms are lengthy exacerbations or "flares" of the illness after ordinary minor physical or mental activity, known as post-exertional malaise (PEM);[13][14] greatly diminished capacity to accomplish tasks that were routine before the illness; and sleep disturbances.[13][15][1][5][2]: 7 Orthostatic intolerance (difficulty sitting and standing upright) and cognitive dysfunction are also diagnostic. Frequently and variably, other common symptoms occur involving numerous body systems, and chronic pain is common.[15][16] The unexplained and often incapacitating fatigue in CFS is different from that caused by normal strenuous ongoing exertion, is not significantly relieved by rest, and is not due to a previous medical condition.[15] Diagnosis is based on the person's symptoms because no confirmed diagnostic test is available.[17]
"""
https://en.wikipedia.org/wiki/Controversies_related_to_chronic_fatigue_syndrome
"""
Chronic fatigue syndrome (CFS), also called myalgic encephalomyelitis (ME) or ME/CFS, is a complex, debilitating, long-term medical condition. The causes and mechanisms of the disease are not yet fully understood. [12] Distinguishing core symptoms are lengthy exacerbations or "flares" of the illness after ordinary minor physical or mental activity, known as post-exertional malaise (PEM);[13][14] greatly diminished capacity to accomplish tasks that were routine before the illness; and sleep disturbances.[13][15][1][5][2]: 7 Orthostatic intolerance (difficulty sitting and standing upright) and cognitive dysfunction are also diagnostic. Frequently and variably, other common symptoms occur involving numerous body systems, and chronic pain is common.[15][16] The unexplained and often incapacitating fatigue in CFS is different from that caused by normal strenuous ongoing exertion, is not significantly relieved by rest, and is not due to a previous medical condition.[15] Diagnosis is based on the person's symptoms because no confirmed diagnostic test is available.[17]
"""
https://en.wikipedia.org/wiki/Controversies_related_to_chronic_fatigue_syndrome
¶Meningoencephalitis
https://en.wikipedia.org/wiki/Meningoencephalitis
"Causative organisms include protozoans, viral and bacterial pathogens."
https://en.wikipedia.org/wiki/Controversies_related_to_chronic_fatigue_syndrome
"""
Protozoal
Animal
Halicephalobus gingivalis
This nematode is an exceptionally rare cause of meningoencephalitis.[19]
____________
Other/multiple
Other causes include granulomatous meningoencephalitis and vasculitis. The fungus, Cryptococcus neoformans, can be symptomatically manifested within the CNS as meningoencephalitis with hydrocephalus being a very characteristic finding due to the unique thick polysaccharide capsule of the organism.[citation needed]
"""
_______ TREAT
"""
Antiviral therapy, such as acyclovir and ganciclovir, work best when applied as early as possible. May also be treated with interferon as an immune therapy. Symptomatic therapy can be applied as needed
"""
https://en.wikipedia.org/wiki/Meningoencephalitis
"Causative organisms include protozoans, viral and bacterial pathogens."
https://en.wikipedia.org/wiki/Controversies_related_to_chronic_fatigue_syndrome
"""
Protozoal
- Naegleria fowleri (percolozoa)
- Trypanosoma brucei (euglenozoa)
- Toxoplasma gondii (apicomplexa)
Animal
Halicephalobus gingivalis
This nematode is an exceptionally rare cause of meningoencephalitis.[19]
____________
Other/multiple
Other causes include granulomatous meningoencephalitis and vasculitis. The fungus, Cryptococcus neoformans, can be symptomatically manifested within the CNS as meningoencephalitis with hydrocephalus being a very characteristic finding due to the unique thick polysaccharide capsule of the organism.[citation needed]
"""
_______ TREAT
"""
Antiviral therapy, such as acyclovir and ganciclovir, work best when applied as early as possible. May also be treated with interferon as an immune therapy. Symptomatic therapy can be applied as needed
"""
¶Antibiotic-associated diarrhea (AAD)
https://en.wikipedia.org/wiki/Antibiotic-associated_diarrhea
"""
Antibiotic-associated diarrhea (AAD) results from an imbalance in the colonic microbiota caused by antibiotics. Microbiotal alteration changes carbohydrate metabolism with decreased short-chain fatty acid absorption and an osmotic diarrhea as a result. Another consequence of antibiotic therapy leading to diarrhea is overgrowth of potentially pathogenic organisms such as Clostridium difficile. It is defined as frequent loose and watery stools with no other complications.[1]
"""
https://en.wikipedia.org/wiki/Antibiotic-associated_diarrhea
"""
Antibiotic-associated diarrhea (AAD) results from an imbalance in the colonic microbiota caused by antibiotics. Microbiotal alteration changes carbohydrate metabolism with decreased short-chain fatty acid absorption and an osmotic diarrhea as a result. Another consequence of antibiotic therapy leading to diarrhea is overgrowth of potentially pathogenic organisms such as Clostridium difficile. It is defined as frequent loose and watery stools with no other complications.[1]
"""
¶Perioral dermatitis
https://en.wikipedia.org/wiki/Perioral_dermatitis
"""
Perioral dermatitis, also known as periorificial dermatitis, is a common type of skin rash. Symptoms include multiple small (1–2 mm) bumps and blisters sometimes with background redness and scale, localized to the skin around the mouth and nostrils. Less commonly the eyes and genitalia may be involved.[2] It can be persistent or recurring and resembles particularly rosacea and to some extent acne and allergic dermatitis. The term "dermatitis" is a misnomer because this is not an eczematous process.[3]
The cause is unclear.[1] Topical steroids are associated with the condition and moisturizers and cosmetics may contribute.[3] The underlying mechanism may involve blockage of the skin surface followed by subsequent excessive growth of skin flora. Fluoridated toothpaste and some micro-organisms including Candida may also worsen the condition, but their roles in this condition is unclear.[4] It is considered a disease of the hair follicle with biopsy samples showing microscopic changes around the hair follicle. Diagnosis is based on symptoms.[4]
"""
https://en.wikipedia.org/wiki/Perioral_dermatitis
"""
Perioral dermatitis, also known as periorificial dermatitis, is a common type of skin rash. Symptoms include multiple small (1–2 mm) bumps and blisters sometimes with background redness and scale, localized to the skin around the mouth and nostrils. Less commonly the eyes and genitalia may be involved.[2] It can be persistent or recurring and resembles particularly rosacea and to some extent acne and allergic dermatitis. The term "dermatitis" is a misnomer because this is not an eczematous process.[3]
The cause is unclear.[1] Topical steroids are associated with the condition and moisturizers and cosmetics may contribute.[3] The underlying mechanism may involve blockage of the skin surface followed by subsequent excessive growth of skin flora. Fluoridated toothpaste and some micro-organisms including Candida may also worsen the condition, but their roles in this condition is unclear.[4] It is considered a disease of the hair follicle with biopsy samples showing microscopic changes around the hair follicle. Diagnosis is based on symptoms.[4]
"""
¶Water contamination (bacteriological, pesticides, pharmaceutical, heavy metals, etc)
(SLO)
https://www.nlzoh.si/storitve/vode/pitne-vode/
(SLO)
https://www.nlzoh.si/storitve/vode/pitne-vode/
¶tetanus
[!!¶] check for vaccinations
"""
Use of aqueous iodine or 2% glutaraldehyde at pH 7.5 to 8.5 kills spores within 3 hours; autoclaving at 120° C and 15 psi destroys them within 15 to 20 minutes. The most common source of environmental exposure to C. tetani bacilli and spores is soil, where the organism is widely but variably distributed.
"""
[!!¶] check for vaccinations
"""
Use of aqueous iodine or 2% glutaraldehyde at pH 7.5 to 8.5 kills spores within 3 hours; autoclaving at 120° C and 15 psi destroys them within 15 to 20 minutes. The most common source of environmental exposure to C. tetani bacilli and spores is soil, where the organism is widely but variably distributed.
"""
¶TICKS/BACTERIA— Ticks→ HGA (Anaplasmosis)
https://en.wikipedia.org/wiki/Human_granulocytic_anaplasmosis
"""
Human granulocytic anaplasmosis (HGA) is a tick-borne, infectious disease caused by Anaplasma phagocytophilum, an obligate intracellular bacterium that is typically transmitted to humans by ticks of the Ixodes ricinus species complex, including Ixodes scapularis and Ixodes pacificus in North America. These ticks also transmit Lyme disease and other tick-borne diseases.[3]
The bacteria infect white blood cells called neutrophils, causing changes in gene expression that prolong the life of these otherwise short-lived cells.[4]
[...]
Doxycycline is the treatment of choice. If anaplasmosis is suspected, treatment should not be delayed while waiting for a definitive laboratory confirmation, as prompt doxycycline therapy has been shown to improve outcomes.[
"""
https://www.canada.ca/en/public-health/services/diseases/ticks-tick-borne-diseases/anaplasmosis.html#a1
"The first symptoms can appear within 5 to 21 days. [...] Anaplasmosis is treated with antibiotics. The earlier you receive treatment for anaplasmosis, the greater the chance of a successful recovery."
__________________________________________
Related: DOGS ONLY version
https://en.wikipedia.org/wiki/Anaplasmosis
https://en.wikipedia.org/wiki/Human_granulocytic_anaplasmosis
"""
Human granulocytic anaplasmosis (HGA) is a tick-borne, infectious disease caused by Anaplasma phagocytophilum, an obligate intracellular bacterium that is typically transmitted to humans by ticks of the Ixodes ricinus species complex, including Ixodes scapularis and Ixodes pacificus in North America. These ticks also transmit Lyme disease and other tick-borne diseases.[3]
The bacteria infect white blood cells called neutrophils, causing changes in gene expression that prolong the life of these otherwise short-lived cells.[4]
[...]
Doxycycline is the treatment of choice. If anaplasmosis is suspected, treatment should not be delayed while waiting for a definitive laboratory confirmation, as prompt doxycycline therapy has been shown to improve outcomes.[
"""
https://www.canada.ca/en/public-health/services/diseases/ticks-tick-borne-diseases/anaplasmosis.html#a1
"The first symptoms can appear within 5 to 21 days. [...] Anaplasmosis is treated with antibiotics. The earlier you receive treatment for anaplasmosis, the greater the chance of a successful recovery."
__________________________________________
Related: DOGS ONLY version
https://en.wikipedia.org/wiki/Anaplasmosis
¶TICKS— Ehrlichiosis
Related to Anaplasmosis
(!) USA-only
Ehrlichiosis
https://en.wikipedia.org/wiki/Ehrlichiosis
"""
Ehrlichiosis is a tick-borne[3] bacterial infection,[4] caused by bacteria of the family Anaplasmataceae, genera Ehrlichia and Anaplasma. These obligate intracellular bacteria infect and kill white blood cells.
The average reported annual incidence is on the order of 2.3 cases per million people.[5]
"""
Related to Anaplasmosis
(!) USA-only
Ehrlichiosis
https://en.wikipedia.org/wiki/Ehrlichiosis
"""
Ehrlichiosis is a tick-borne[3] bacterial infection,[4] caused by bacteria of the family Anaplasmataceae, genera Ehrlichia and Anaplasma. These obligate intracellular bacteria infect and kill white blood cells.
The average reported annual incidence is on the order of 2.3 cases per million people.[5]
"""
¶TICKS— Rickettsiosis (Spotted Fever Group)
The Rickettsiae are a diverse group of bacteria some of which can be transmitted to humans via the bites of fleas, lice, ticks or mites.
Fast Transmission Time(!)
Transmission can occur more quickly, often within 6 to 10 hours of attachment. Some studies suggest that transmission can happen even sooner.
↓
Doxycycline has been used in the treatment of rickettsial infection
https://en.wikipedia.org/wiki/Rickettsiosis
The Rickettsiae are a diverse group of bacteria some of which can be transmitted to humans via the bites of fleas, lice, ticks or mites.
Fast Transmission Time(!)
Transmission can occur more quickly, often within 6 to 10 hours of attachment. Some studies suggest that transmission can happen even sooner.
↓
Doxycycline has been used in the treatment of rickettsial infection
https://en.wikipedia.org/wiki/Rickettsiosis
¶PLANTS— (spotted lanternfly)
https://en.wikipedia.org/wiki/Spotted_lanternfly
https://en.wikipedia.org/wiki/File:Potential_Global_Distribution_of_Spotted_Lanternfly.jpg
distribution viability
https://en.wikipedia.org/wiki/Spotted_lanternfly
https://en.wikipedia.org/wiki/File:Potential_Global_Distribution_of_Spotted_Lanternfly.jpg
distribution viability
¶e.coli
basics, causes, etc
* present in stool of infected
* hand-to-mouth pathway:
(infected kaka touches food sometimes in the processing, which is not sterilized properly)
* contagious in this way!
* causes Epididymitis (TESTICULAR SWELLING) in advanced stage
———————
https://www.healthline.com/health/contagious-e-coli#prevention
"""
Infectious E. coli bacteria can be spread from humans and animals. The most common ways it spreads are:
https://www.urologyhealth.org/urology-a-z/e/epididymitis-and-orchitis
—————— case @cuba
#medical [!→]
"i need nitrofurantoina"
how do you get it?:
"i need to find groups in telegram"
https://en.wikipedia.org/wiki/Nitrofurantoin
————— treatment
"""
According to [7], E. coli is highly resistant to ampicillin, amoxicillin, tetracycline and trimethoprim & sulfamethoxazole
"""
"""
In severe infection, piperacillin and tazobactam, imipenem and cilastatin, or meropenem may be used. Combination therapy with antibiotics that cover E coli plus an antianaerobe can also be used (eg, levofloxacin plus clindamycin or metronidazole).Feb 11, 2019
"""
basics, causes, etc
* present in stool of infected
* hand-to-mouth pathway:
(infected kaka touches food sometimes in the processing, which is not sterilized properly)
* contagious in this way!
* causes Epididymitis (TESTICULAR SWELLING) in advanced stage
———————
https://www.healthline.com/health/contagious-e-coli#prevention
"""
Infectious E. coli bacteria can be spread from humans and animals. The most common ways it spreads are:
- eating undercooked or raw meat
- eating contaminated, raw fruits and vegetables
- drinking unpasteurized milk
- swimming in or drinking contaminated water
- contact with a person who has poor hygiene and doesn’t wash their hands regularly
- contact with infected animals
https://www.urologyhealth.org/urology-a-z/e/epididymitis-and-orchitis
—————— case @cuba
#medical [!→]
"i need nitrofurantoina"
how do you get it?:
"i need to find groups in telegram"
https://en.wikipedia.org/wiki/Nitrofurantoin
————— treatment
"""
According to [7], E. coli is highly resistant to ampicillin, amoxicillin, tetracycline and trimethoprim & sulfamethoxazole
"""
"""
In severe infection, piperacillin and tazobactam, imipenem and cilastatin, or meropenem may be used. Combination therapy with antibiotics that cover E coli plus an antianaerobe can also be used (eg, levofloxacin plus clindamycin or metronidazole).Feb 11, 2019
"""
¶CUBA— Sand fleas (Tunga penetrans) → tungiasis
First there are "FALSE", colloquial "SAND FLEAS":
"""
The most common and least dangerous of all the organisms that people call “sand fleas” are actually crustaceans. So, they aren’t fleas or even insects. They’re in the same family as crabs and lobsters. People only call them “fleas” because they hop and jump. You might also hear them referred to as sand hoppers, beach fleas or beach hoppers. These creatures might cause red, itchy bumps on your skin, but the irritation usually goes away in a few days.
"""
https://my.clevelandclinic.org/health/diseases/24458-sand-flea-bites
"""
True sand fleas are the Tunga penetrans, also called the chigoe flea or jigger flea. These fleas (the smallest known flea) can bore holes into your skin. They may cause a parasitic infection called tungiasis (sand flea disease) that can lead to severe inflammation and skin lesions (wounds). Chigoe fleas are typically in tropical climates such as Central America, South America, Africa, the Caribbean and the West Indies. They’re rare in the U.S.
(...)
They live in humid conditions. So, if you’re walking barefoot on the beach, playing in the sand or wading in warm, shallow water, you may get bites.
(...)
Both common sand flea bites and chigoe flea bites tend to occur on your ankles and feet.
"""
----------------------------
"""
Erma Rodriguez Kraft
The sand flea can live inside your skin, growing bigger with its eggs and your blood, for up to six weeks
Tungiasis is caused by female sand fleas, which burrow into the skin and lay eggs.
Tungiasis can cause abscesses, secondary infections, gangrene and disfigurement. Please see your Dr
"""
https://www.who.int/news-room/fact-sheets/detail/tungiasis
"""
Tungiasis is a cutaneous parasitosis caused by infection with the female sand flea Tunga penetrans (and T. trimamillatain some areas). It is also commonly known as pulga de areia, niguá, pique, bicho do pé, bichodo porco or jatecuba, and, in English-speaking countries, as jigger, sand flea or chigoe. Tungiasis is a zoonosis that affects humans and animals alike.
[...]
The flea typically lives for 4–6 weeks, after which the eggs are expelled and fall to the ground. The toes, sole, lateral rim of the foot and heel are common sites, and 99% of all lesions occur on the feet. Considerable itching and pain occur as the female fleas develop fully and increase their body volume by a factor of 2000 within one week. Bacterial infections in the lesions can cause abscesses, suppuration or lymphangitis. Multiple lesions and intense local inflammation exacerbate the pain and restrict mobility.
[...]
Several mammalian species can act as reservoirs for human infection. In rural areas, these are predominantly pigs and bovines; in resource-poor urban communities, dogs, cats and rats. In some areas, infection can be transmitted without an animal reservoir when skin comes into contact with soil or a floor where adult sand fleas have developed. Infection often takes place inside the house, the surrounding area or in classrooms without sealed floors.
"""
————— secondary problems
"""
In endemic areas, the standard treatment is surgical extraction of burrowed sand fleas, which is usually done by the patients themselves or a caregiver. Embedded parasites are removed under non-sterile conditions using instruments such as sticks, hair pins, sewing needles or scissors. The procedure is painful and poorly tolerated by children. Removing the fleas can cause local inflammation if the parasite ruptures and introduce pathogenic bacteria, leading to superinfection of the sore. The instrument is often subsequently used on several persons, which risks transmission of diseases such as hepatitis B virus (HBV), hepatitis C virus (HCV) or HIV.
[...]
Metrifonate, thiabendazole and ivermectin have been tested as topical applications; however, none proved to be sufficiently effective1. The topical application of a two-component dimeticone with a defined viscosity, as found in treatments for headlice, is highly effective2,3.
""""
————— curing
""""
The regular application of a repellent based on coconut oil effectively prevents the fleas from penetrating the skin. When the repellent is applied twice daily on the feet, tungiasis-associated morbidity rapidly decreases and approaches zero after 8–10 weeks 4. Even if applied intermittently, the reduction of morbidity is significant.
"""
First there are "FALSE", colloquial "SAND FLEAS":
"""
The most common and least dangerous of all the organisms that people call “sand fleas” are actually crustaceans. So, they aren’t fleas or even insects. They’re in the same family as crabs and lobsters. People only call them “fleas” because they hop and jump. You might also hear them referred to as sand hoppers, beach fleas or beach hoppers. These creatures might cause red, itchy bumps on your skin, but the irritation usually goes away in a few days.
"""
https://my.clevelandclinic.org/health/diseases/24458-sand-flea-bites
"""
True sand fleas are the Tunga penetrans, also called the chigoe flea or jigger flea. These fleas (the smallest known flea) can bore holes into your skin. They may cause a parasitic infection called tungiasis (sand flea disease) that can lead to severe inflammation and skin lesions (wounds). Chigoe fleas are typically in tropical climates such as Central America, South America, Africa, the Caribbean and the West Indies. They’re rare in the U.S.
(...)
They live in humid conditions. So, if you’re walking barefoot on the beach, playing in the sand or wading in warm, shallow water, you may get bites.
(...)
Both common sand flea bites and chigoe flea bites tend to occur on your ankles and feet.
"""
----------------------------
"""
The sand flea can live inside your skin, growing bigger with its eggs and your blood, for up to six weeks
Tungiasis is caused by female sand fleas, which burrow into the skin and lay eggs.
Tungiasis can cause abscesses, secondary infections, gangrene and disfigurement. Please see your Dr
"""
https://www.who.int/news-room/fact-sheets/detail/tungiasis
"""
- Tungiasis is caused by female sand fleas, which burrow into the skin and lay eggs.
- Tungiasis can cause abscesses, secondary infections, gangrene and disfigurement.
- The disease is found in most tropical and subtropical areas of the world; the poorest people carry the highest burden of the disease.
- Both animals and humans are susceptible.
Tungiasis is a cutaneous parasitosis caused by infection with the female sand flea Tunga penetrans (and T. trimamillatain some areas). It is also commonly known as pulga de areia, niguá, pique, bicho do pé, bichodo porco or jatecuba, and, in English-speaking countries, as jigger, sand flea or chigoe. Tungiasis is a zoonosis that affects humans and animals alike.
[...]
The flea typically lives for 4–6 weeks, after which the eggs are expelled and fall to the ground. The toes, sole, lateral rim of the foot and heel are common sites, and 99% of all lesions occur on the feet. Considerable itching and pain occur as the female fleas develop fully and increase their body volume by a factor of 2000 within one week. Bacterial infections in the lesions can cause abscesses, suppuration or lymphangitis. Multiple lesions and intense local inflammation exacerbate the pain and restrict mobility.
[...]
Several mammalian species can act as reservoirs for human infection. In rural areas, these are predominantly pigs and bovines; in resource-poor urban communities, dogs, cats and rats. In some areas, infection can be transmitted without an animal reservoir when skin comes into contact with soil or a floor where adult sand fleas have developed. Infection often takes place inside the house, the surrounding area or in classrooms without sealed floors.
"""
————— secondary problems
"""
In endemic areas, the standard treatment is surgical extraction of burrowed sand fleas, which is usually done by the patients themselves or a caregiver. Embedded parasites are removed under non-sterile conditions using instruments such as sticks, hair pins, sewing needles or scissors. The procedure is painful and poorly tolerated by children. Removing the fleas can cause local inflammation if the parasite ruptures and introduce pathogenic bacteria, leading to superinfection of the sore. The instrument is often subsequently used on several persons, which risks transmission of diseases such as hepatitis B virus (HBV), hepatitis C virus (HCV) or HIV.
[...]
Metrifonate, thiabendazole and ivermectin have been tested as topical applications; however, none proved to be sufficiently effective1. The topical application of a two-component dimeticone with a defined viscosity, as found in treatments for headlice, is highly effective2,3.
""""
————— curing
""""
The regular application of a repellent based on coconut oil effectively prevents the fleas from penetrating the skin. When the repellent is applied twice daily on the feet, tungiasis-associated morbidity rapidly decreases and approaches zero after 8–10 weeks 4. Even if applied intermittently, the reduction of morbidity is significant.
"""
¶Tuberculosis (TBC)
https://arstechnica.com/science/2023/02/us-woman-has-walked-around-with-untreated-tb-for-over-a-year-now-faces-jail/
there's idiotic people running around with it,
[!!] involuntary isolation rules/laws/provisions
https://arstechnica.com/science/2023/02/us-woman-has-walked-around-with-untreated-tb-for-over-a-year-now-faces-jail/
there's idiotic people running around with it,
[!!] involuntary isolation rules/laws/provisions
¶FUNGAL— Fungal meningytis (via fungal spores)
For example, in:
* pigeon droppings
* ###
via https://apnews.com/article/caribbean-mexico-city-health-medication-92822e20d3dd647b8e929a3c066f7efa
(>30 dead in fungal contaminated morphine)
... similar case mentions "Fusarium solani"
###
https://www.cdc.gov/meningitis/fungal.html
"""
Fungal meningitis can develop after a fungal infection spreads from somewhere else in the body to the brain or spinal cord.
Some causes of fungal meningitis include Cryptococcus, Histoplasma, Blastomyces, Coccidioides, and Candida.
Many fungi that can cause meningitis live in the environment:
"""
prevention?
People with weak immune systems should [...]
"""
This is especially true if they live in a geographic region where fungi like Histoplasma, Coccidioides, or Blastomyces exist.
"""
_____ testing
https://www.publichealthontario.ca/en/Laboratory-Services/Test-Information-Index/Cryptococcus-Direct-Blood-CSF
"""
This page provides information on cryptococcal antigen Latex agglutination testing at Public Health Ontario’s (PHO) laboratory. The causative agent(s) of cryptococcosis is Cryptococcus neoformans. This page is for information specific to Antigen Latex Agglutination testing. Antibody testing is not available at PHO’s laboratory.
The Cryptococcal Antigen Latex Agglutination System (CALAS) is a qualitative and semi-quantitative test system for the detection of capsular polysaccharide antigens of Cryptococcus neoformans in serum and cerebrospinal fluid (CSF).
"""
https://pubmed.ncbi.nlm.nih.gov/32829406/
"""
Abstract
Cryptococcal antigen (CrAg) detection could direct the timely initiation of antifungal therapy. We searched MEDLINE and Embase for studies where CrAg detection in serum/cerebrospinal fluid (CSF) and CSF fungal culture were done on adults living with human immunodeficiency virus (HIV) who had suspected cryptococcal meningitis (CM). With Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2), we evaluated the risk of bias in 11 included studies with 3600 participants, and used a random-effects meta-analysis to obtain summary sensitivity and specificity of serum and CSF CrAg, as well as agreement between CSF CrAg and CSF culture. Summary sensitivity and specificity of serum CrAg were 99.7% (97.4-100) and 94.1% (88.3-98.1), respectively, and summary sensitivity and specificity of CSF CrAg were 98.8% (96.2-99.6) and 99.3% (96.7-99.9), respectively. Agreement between CSF CrAg and CSF culture was 98% (97-99). In adults living with HIV who have CM symptoms, serum CrAg negativity may rule out CM, while positivity should prompt induction antifungal therapy if lumbar puncture is not feasible. In a first episode of CM, CSF CrAg positivity is diagnostic.
Keywords: antigen; cryptococcus; diagnosis; lateral flow assay; latex agglutination.
"""
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4858186/
"""
Over the last decade, an upsurge in both the frequency and severity of fungal infections due to the HIV/AIDS epidemic and the use of immunosuppressive therapy has occurred. Even diagnostic methods like culture and microscopy, which have low sensitivity and longer turn-around-times are not widely available, leading to delays in timely antifungal therapy and detrimental patient outcomes. The evolution of cryptococcal antigen (CrAg) testing to develop inexpensive and more sensitive methods to detect cryptococcal antigen is significant. These newer tests employ immunoassays as part of point-of-care platforms, which do not require complex laboratory infrastructure and they have the potential to detect early disease and reduce time to diagnosis of cryptococcal infection. Advocacy for widely available and efficacious life-saving antifungal treatment should be the only remaining challenge.
Keywords: Cryptococcus, antigen, testing, lateral flow, assay, HIV, diagnosis, thermal contrast, Fungus, cryptococcal disease, cryptococcal meningitis
[...]
Infection with the human immunodeficiency virus (HIV) and increased use of immunosuppressive therapy have led to an increase in both the frequency and severity of fungal infections [1]•. Cryptococcus neoformans and Cryptococcus gatti are responsible for an estimated 700,000 cases of cryptococcal meningitis in sub Saharan Africa [2] and 7,800 cases of cryptococcal meningitis in North America in 2006 respectively [3]. Mortality from cryptococcal disease remains high even in the era of ART. Early diagnosis of cryptococcal infection is critical to improving clinical outcomes.
A notable increase in the prevalence of cryptococcal meningitis in the last decade has not been matched by improved diagnostics in resource limited settings where most of the infections occur. The low sensitivity of older test methods and delay in obtaining results has driven research for cheaper and more widely available sensitive diagnostics.
"""
________________
https://kvarkadabra.net/2024/05/spol-raziskave-gliv
"""
Najmanj znana izmed navedenih glivni bolezni je bila blastomikoza, ki jo je prepoznalo le 4 % tistih, ki so sodelovali v anketi, sledile so aspergiloza, histoplazmoza, kokcidioidomikoza in kriptokokoza, najbolj prepoznana pa je bila kandidoza (25 %).
"""
For example, in:
* pigeon droppings
* ###
via https://apnews.com/article/caribbean-mexico-city-health-medication-92822e20d3dd647b8e929a3c066f7efa
(>30 dead in fungal contaminated morphine)
... similar case mentions "Fusarium solani"
###
https://www.cdc.gov/meningitis/fungal.html
"""
Fungal meningitis can develop after a fungal infection spreads from somewhere else in the body to the brain or spinal cord.
Some causes of fungal meningitis include Cryptococcus, Histoplasma, Blastomyces, Coccidioides, and Candida.
Many fungi that can cause meningitis live in the environment:
- Cryptococcus lives in the environment throughout the world.
- Histoplasma lives in the environment, particularly in soil that contains large amounts of bird or bat droppings. In the United States, the fungus mainly lives in the central and eastern states. →→ https://www.cdc.gov/fungal/diseases/histoplasmosis/index.html
- Blastomyces lives in moist soil and in decaying wood and leaves. In the United States, the fungus mainly lives in midwestern, south central, and southeastern states.
- Coccidioides lives in the soil in the southwestern United States, south-central Washington State, and parts of Mexico and Central and South America.
"""
prevention?
People with weak immune systems should [...]
"""
This is especially true if they live in a geographic region where fungi like Histoplasma, Coccidioides, or Blastomyces exist.
"""
_____ testing
https://www.publichealthontario.ca/en/Laboratory-Services/Test-Information-Index/Cryptococcus-Direct-Blood-CSF
"""
This page provides information on cryptococcal antigen Latex agglutination testing at Public Health Ontario’s (PHO) laboratory. The causative agent(s) of cryptococcosis is Cryptococcus neoformans. This page is for information specific to Antigen Latex Agglutination testing. Antibody testing is not available at PHO’s laboratory.
The Cryptococcal Antigen Latex Agglutination System (CALAS) is a qualitative and semi-quantitative test system for the detection of capsular polysaccharide antigens of Cryptococcus neoformans in serum and cerebrospinal fluid (CSF).
"""
https://pubmed.ncbi.nlm.nih.gov/32829406/
"""
Abstract
Cryptococcal antigen (CrAg) detection could direct the timely initiation of antifungal therapy. We searched MEDLINE and Embase for studies where CrAg detection in serum/cerebrospinal fluid (CSF) and CSF fungal culture were done on adults living with human immunodeficiency virus (HIV) who had suspected cryptococcal meningitis (CM). With Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2), we evaluated the risk of bias in 11 included studies with 3600 participants, and used a random-effects meta-analysis to obtain summary sensitivity and specificity of serum and CSF CrAg, as well as agreement between CSF CrAg and CSF culture. Summary sensitivity and specificity of serum CrAg were 99.7% (97.4-100) and 94.1% (88.3-98.1), respectively, and summary sensitivity and specificity of CSF CrAg were 98.8% (96.2-99.6) and 99.3% (96.7-99.9), respectively. Agreement between CSF CrAg and CSF culture was 98% (97-99). In adults living with HIV who have CM symptoms, serum CrAg negativity may rule out CM, while positivity should prompt induction antifungal therapy if lumbar puncture is not feasible. In a first episode of CM, CSF CrAg positivity is diagnostic.
Keywords: antigen; cryptococcus; diagnosis; lateral flow assay; latex agglutination.
"""
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4858186/
"""
Over the last decade, an upsurge in both the frequency and severity of fungal infections due to the HIV/AIDS epidemic and the use of immunosuppressive therapy has occurred. Even diagnostic methods like culture and microscopy, which have low sensitivity and longer turn-around-times are not widely available, leading to delays in timely antifungal therapy and detrimental patient outcomes. The evolution of cryptococcal antigen (CrAg) testing to develop inexpensive and more sensitive methods to detect cryptococcal antigen is significant. These newer tests employ immunoassays as part of point-of-care platforms, which do not require complex laboratory infrastructure and they have the potential to detect early disease and reduce time to diagnosis of cryptococcal infection. Advocacy for widely available and efficacious life-saving antifungal treatment should be the only remaining challenge.
Keywords: Cryptococcus, antigen, testing, lateral flow, assay, HIV, diagnosis, thermal contrast, Fungus, cryptococcal disease, cryptococcal meningitis
[...]
Infection with the human immunodeficiency virus (HIV) and increased use of immunosuppressive therapy have led to an increase in both the frequency and severity of fungal infections [1]•. Cryptococcus neoformans and Cryptococcus gatti are responsible for an estimated 700,000 cases of cryptococcal meningitis in sub Saharan Africa [2] and 7,800 cases of cryptococcal meningitis in North America in 2006 respectively [3]. Mortality from cryptococcal disease remains high even in the era of ART. Early diagnosis of cryptococcal infection is critical to improving clinical outcomes.
A notable increase in the prevalence of cryptococcal meningitis in the last decade has not been matched by improved diagnostics in resource limited settings where most of the infections occur. The low sensitivity of older test methods and delay in obtaining results has driven research for cheaper and more widely available sensitive diagnostics.
"""
________________
https://kvarkadabra.net/2024/05/spol-raziskave-gliv
"""
Najmanj znana izmed navedenih glivni bolezni je bila blastomikoza, ki jo je prepoznalo le 4 % tistih, ki so sodelovali v anketi, sledile so aspergiloza, histoplazmoza, kokcidioidomikoza in kriptokokoza, najbolj prepoznana pa je bila kandidoza (25 %).
"""
¶FUNGAL— Blastomycosis (lungs, skin, brain)
https://en.wikipedia.org/wiki/Blastomycosis
"""
Blastomycosis, also known as Gilchrist's disease, is a fungal infection, typically of the lungs, which can spread to brain, stomach, intestine and skin, where it appears as crusting purplish warty plaques with a roundish bumpy edge and central depression.[2][7] Around half of people with the disease have symptoms, which can include fever, cough, night sweats, muscle pains, weight loss, chest pain, and fatigue.[5] Symptoms usually develop between three weeks and three months after breathing in the spores.[5] In 25% to 40% of cases, the infection also spreads to other parts of the body, such as the skin, bones or central nervous system.[8] Although blastomycosis is especially dangerous for those with weak immune systems, most people diagnosed with blastomycosis have healthy immune systems.[8]
"""
https://vseozdravju.si/bolezni/blastomikoza/
"""
Blastomikoza je glivična okužba, ki jo povzroča gliva Blastomyces dermatitidis. Ta gliva je naravno prisotna v nekaterih delih Severne Amerike, predvsem v tleh in gnoju. Okužba lahko prizadene ljudi in živali.
[...]
Če živite ali potujete v območjih, kjer je prisotna gliva Blastomyces dermatitidis, je pomembno, da se zaščitite pred okužbo:
https://en.wikipedia.org/wiki/Blastomycosis
"""
Blastomycosis, also known as Gilchrist's disease, is a fungal infection, typically of the lungs, which can spread to brain, stomach, intestine and skin, where it appears as crusting purplish warty plaques with a roundish bumpy edge and central depression.[2][7] Around half of people with the disease have symptoms, which can include fever, cough, night sweats, muscle pains, weight loss, chest pain, and fatigue.[5] Symptoms usually develop between three weeks and three months after breathing in the spores.[5] In 25% to 40% of cases, the infection also spreads to other parts of the body, such as the skin, bones or central nervous system.[8] Although blastomycosis is especially dangerous for those with weak immune systems, most people diagnosed with blastomycosis have healthy immune systems.[8]
"""
https://vseozdravju.si/bolezni/blastomikoza/
"""
Blastomikoza je glivična okužba, ki jo povzroča gliva Blastomyces dermatitidis. Ta gliva je naravno prisotna v nekaterih delih Severne Amerike, predvsem v tleh in gnoju. Okužba lahko prizadene ljudi in živali.
[...]
Če živite ali potujete v območjih, kjer je prisotna gliva Blastomyces dermatitidis, je pomembno, da se zaščitite pred okužbo:
- Izogibajte se vdihavanju prsti ali peska v okuženih območjih.
- Nosite masko ali respirator pri delu, ki lahko povzroči izpostavljenost glivi.
- Izogibajte se stiku z gnojem ali odpadki živali.
- Po delu ali aktivnostih na prostem si temeljito umijte roke in oblačila.
¶Fire ants (cuba: santanilla/santanica)
###
they don't bite, but spray stuff on you
wash it off!
### moo: "i learned to live with it ... they are everywhere ... in all the trees ..."
In Cuba, it's an invasive pest!
https://www.ecured.cu/Santanilla
"""
Wasmannia auropunctata . Pequeña hormiga de fuego como también suele llamársele, es culpada por la reducción de la diversidad de especies, la reducción de la abundancia total de insectos voladores que viven en los árboles, y la eliminación de las poblaciones de arácnidos. También es conocido por sus dolorosas picaduras.
"""
Good advice to get rid of
https://fuerteventura.click/Thread-Ants-and-how-to-control-edadicate-them?page=2
* spill sugar
* see their entry
* block + sanitize with KH7
###
they don't bite, but spray stuff on you
wash it off!
In Cuba, it's an invasive pest!
https://www.ecured.cu/Santanilla
"""
Wasmannia auropunctata . Pequeña hormiga de fuego como también suele llamársele, es culpada por la reducción de la diversidad de especies, la reducción de la abundancia total de insectos voladores que viven en los árboles, y la eliminación de las poblaciones de arácnidos. También es conocido por sus dolorosas picaduras.
"""
Good advice to get rid of
https://fuerteventura.click/Thread-Ants-and-how-to-control-edadicate-them?page=2
* spill sugar
* see their entry
* block + sanitize with KH7
¶iron/sulfur bacteria (not problematic)
the gelly stuff found in toilet water tanks
https://extension.psu.edu/iron-and-sulfur-bacteria-a-slimy-problem
"""
Iron bacteria typically exist on top of the ground, either in soil or surface water. While some iron bacteria may occur naturally in groundwater, more often they are introduced into water wells during well construction or maintenance. These bacteria can then be introduced into the well if well components are laid on soil containing iron bacteria, if contaminated surface water is used as drilling water, if drilling equipment is contaminated by bacteria, or if poor well construction allows for contamination from flooding, septic systems, or other sources.
[...]
Tastes and odors produced by iron bacteria are described as swampy, musty, or like oil, petroleum, cucumbers, sewage, or rotten vegetation. Iron bacteria can also cause reddish, yellow, brown, or gray deposits or orange or opaque slimy strands inside toilet tanks or orange-colored water. Testing well water for iron and manganese can provide information on the presence of these metals, which could help confirm the likelihood of iron bacteria if aesthetic symptoms are also found. Since sulfur-reducing bacteria result in the production of hydrogen sulfide gas, the best indication of a sulfur bacteria problem is the rotten-egg odor; however, these bacteria can also produce a dark-colored slime.
"""
the gelly stuff found in toilet water tanks
https://extension.psu.edu/iron-and-sulfur-bacteria-a-slimy-problem
"""
Iron bacteria typically exist on top of the ground, either in soil or surface water. While some iron bacteria may occur naturally in groundwater, more often they are introduced into water wells during well construction or maintenance. These bacteria can then be introduced into the well if well components are laid on soil containing iron bacteria, if contaminated surface water is used as drilling water, if drilling equipment is contaminated by bacteria, or if poor well construction allows for contamination from flooding, septic systems, or other sources.
[...]
Tastes and odors produced by iron bacteria are described as swampy, musty, or like oil, petroleum, cucumbers, sewage, or rotten vegetation. Iron bacteria can also cause reddish, yellow, brown, or gray deposits or orange or opaque slimy strands inside toilet tanks or orange-colored water. Testing well water for iron and manganese can provide information on the presence of these metals, which could help confirm the likelihood of iron bacteria if aesthetic symptoms are also found. Since sulfur-reducing bacteria result in the production of hydrogen sulfide gas, the best indication of a sulfur bacteria problem is the rotten-egg odor; however, these bacteria can also produce a dark-colored slime.
"""
¶(specific mosquitos) → dengue
https://havanatimes.org/features/cuban-population-on-dengue-fever-alert/
[!!] dengue alerts ... how to monitor live situation?
spreading!
"""
Just a few years ago, they didn’t survive at altitudes greater than 1200 meters above sea level, but now they are wreaking havoc at over 1700 m.
If they could only lay eggs in clean water before, they are now appearing in wastewater and brackish water leaks, especially near the coast, which means their habitat has become more diverse.
"""
serotypes!...
"""
Serotype 2 of dengue fever is the one that is most common in Cuba, although some cases of serotype 1 have also been detected. If you are infected with serotype 1 of the virus, you can get any of the others, as you aren’t immune to them.
“When there are cases of different serotypes in the same person, chances of developing more severe symptoms are greater,” Francisco Duran, the national director of Epidemiology, warned.
"""
re-infections are worse, due to ADE!
https://en.wikipedia.org/wiki/Antibody-dependent_enhancement
"""
ADE may follow when a person who has previously been infected with one serotype becomes infected months or years later with a different serotype, producing higher viremia than in first-time infections. Accordingly, while primary (first) infections cause mostly minor disease (dengue fever) in children, re-infection is more likely to be associated with dengue hemorrhagic fever and/or dengue shock syndrome in both children and adults.[37]
"""
treatment?
"""
There is no antiviral treatment for Dengue fever, and the only approved vaccine–Sanofi's Dengvaxia–can prove risky. Dengvaxia can reduce the severity of Dengue fever in those who have had a prior infection. However, Dengvaxia may increase the risk of severe Dengue in those who have not yet been infected
"""
yipes
---------------------
tamiflu don't help
https://pubmed.ncbi.nlm.nih.gov/34995275/
dengue + covid coinfection ... plus resistance?!
"""
From the above observations, it appeared that pre-exposure to DV may render partial protection against COVID-19 as may be the case in highly dengue endemic regions of the world. This epidemiological observation has now been supported by biological evidences.
"""
https://www.sciencedirect.com/science/article/pii/S2001037020305626
https://havanatimes.org/features/cuban-population-on-dengue-fever-alert/
[!!] dengue alerts ... how to monitor live situation?
spreading!
"""
Just a few years ago, they didn’t survive at altitudes greater than 1200 meters above sea level, but now they are wreaking havoc at over 1700 m.
If they could only lay eggs in clean water before, they are now appearing in wastewater and brackish water leaks, especially near the coast, which means their habitat has become more diverse.
"""
serotypes!...
"""
Serotype 2 of dengue fever is the one that is most common in Cuba, although some cases of serotype 1 have also been detected. If you are infected with serotype 1 of the virus, you can get any of the others, as you aren’t immune to them.
“When there are cases of different serotypes in the same person, chances of developing more severe symptoms are greater,” Francisco Duran, the national director of Epidemiology, warned.
"""
re-infections are worse, due to ADE!
https://en.wikipedia.org/wiki/Antibody-dependent_enhancement
"""
ADE may follow when a person who has previously been infected with one serotype becomes infected months or years later with a different serotype, producing higher viremia than in first-time infections. Accordingly, while primary (first) infections cause mostly minor disease (dengue fever) in children, re-infection is more likely to be associated with dengue hemorrhagic fever and/or dengue shock syndrome in both children and adults.[37]
"""
treatment?
"""
There is no antiviral treatment for Dengue fever, and the only approved vaccine–Sanofi's Dengvaxia–can prove risky. Dengvaxia can reduce the severity of Dengue fever in those who have had a prior infection. However, Dengvaxia may increase the risk of severe Dengue in those who have not yet been infected
"""
yipes
---------------------
tamiflu don't help
https://pubmed.ncbi.nlm.nih.gov/34995275/
dengue + covid coinfection ... plus resistance?!
"""
From the above observations, it appeared that pre-exposure to DV may render partial protection against COVID-19 as may be the case in highly dengue endemic regions of the world. This epidemiological observation has now been supported by biological evidences.
"""
https://www.sciencedirect.com/science/article/pii/S2001037020305626
¶CUBA— Gnats #3
In Cuba: "jejenes"
also: "roedores"
a general word, but in principle, it's ...
Leptoconops bequaerti
http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30192014000500009
"""
An investigation was carried out in Sevilla town, located in the coastal municipality of Guamá, Santiago de Cuba, to identify the species of insects affecting this population, as well as their main breeding sources and the periods of the adults' greater hematophagus activity, for directing efficiently the strategies to control vectors. To achieve this, larvae entomological interviews and captures of mature insects on human bait were carried out. Leptoconops becquaerti (Kieffer) was identified as the species of greater hematophagus activity during daily hours, with more incidence between 09.30 and 11.30 hours. It was concluded that this new report of the province, and particularly of the mentioned site, constitutes a very useful element from the entomological, hygienic-epidemiological points of view, because gnats are important viral encephalitis and other infectious agents transmitters, as phylarias and diverse protozoos.
Key words: Leptoconops bequaerti, gnats, dipteral hematophagus, vectors, insects stings, entomological control.
"""
i suppose "phylarias"→[sic]→filariasis
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/gnat
(from a horse's perspective)
"""
Family Ceratopogonidae
Culicoides spp. (gnats, sandflies, biting midges, ‘punkies’, ‘no-see-ums’) occur throughout the world, and cause severe irritation and hypersensitivity and are important vectors for diseases such as African horse sickness and equine viral arteritis. Different species have different preferred biting patterns and regional information, relating to the species and local climate, is useful in assessing their local significance. Adult Culicoides gnats are blood-sucking parasites and their bites are immediately painful and annoying for the horse. There is a characteristically rapid onset of pruritus, and the development of local papules and wheals at the site. Individual lesions last for several days, and frequent attacks cause almost continuous irritation. The majority of horses in a group are affected when the populations of Culicoides spp. are at their peak. In some enzootic areas in tropical and sub-tropical countries this can be continuous throughout the year. Culicoides spp. are most active at dusk and dawn, with little activity during the heat of the day and the cool of night. The preferred sites vary depending on the species, but the neck and back, the head, and ventral midline are commonly affected. They are also responsible for the development of a very common hypersensitivity disorder known as ‘sweet itch’ and for a ventral midline dermatitis.
"""
———————— TRY 2 (20250621)
<deepseek
"""
In Cuba, the term "jejenes" (also spelled "jején" in singular) refers to small biting midges or sand flies, primarily from two families:
1. Sand Flies (Psychodidae: Lutzomyia spp.)
2. Biting Midges (Ceratopogonidae: Culicoides spp.)
↓↓↓
Must be CULICOIDES !
———————— IDENTIFICATION
https://cjai.biologicalsurvey.ca/articles/jvlfcah-50/#keyEmbed
great resource
↓
[!!*o] Hard to identify, it is a real problem:
"""
Species level identification of Culicoides is difficult for a variety of reasons. Specimen collection is time-consuming and often requires specialized traps and/or equipment particular to each life stage. Observing such tiny organisms requires the use of high magnification, usually a microscope, to see even the most basic characteristics. Furthermore, specimens must also often be slide-mounted to observe diagnostic characters. Morphological identification of Culicoides often depends upon published species descriptions, which vary widely, and are often dated, cryptic, and based on subjective traits (Borkent and Grogan 2009). The identification process requires access to keys and descriptions from multiple sources (Swanson 2012), as well as a high degree of expertise in working with biting midges. The ability to identify Culicoides species is of increasing importance as the current climate crisis affects the distributions of several arthropod species of veterinary importance (Elbers et al. 2015; Vigil et al. 2018).
"""
https://www.mdpi.com/2075-4450/12/5/401
some photos
###
https://www.mdpi.com/2075-4450/12/4/366
nice photo of parts
https://bugguide.net/node/view/19768
###
In Cuba: "jejenes"
also: "roedores"
a general word, but in principle, it's ...
Leptoconops bequaerti
http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30192014000500009
"""
An investigation was carried out in Sevilla town, located in the coastal municipality of Guamá, Santiago de Cuba, to identify the species of insects affecting this population, as well as their main breeding sources and the periods of the adults' greater hematophagus activity, for directing efficiently the strategies to control vectors. To achieve this, larvae entomological interviews and captures of mature insects on human bait were carried out. Leptoconops becquaerti (Kieffer) was identified as the species of greater hematophagus activity during daily hours, with more incidence between 09.30 and 11.30 hours. It was concluded that this new report of the province, and particularly of the mentioned site, constitutes a very useful element from the entomological, hygienic-epidemiological points of view, because gnats are important viral encephalitis and other infectious agents transmitters, as phylarias and diverse protozoos.
Key words: Leptoconops bequaerti, gnats, dipteral hematophagus, vectors, insects stings, entomological control.
"""
i suppose "phylarias"→[sic]→filariasis
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/gnat
(from a horse's perspective)
"""
Family Ceratopogonidae
Culicoides spp. (gnats, sandflies, biting midges, ‘punkies’, ‘no-see-ums’) occur throughout the world, and cause severe irritation and hypersensitivity and are important vectors for diseases such as African horse sickness and equine viral arteritis. Different species have different preferred biting patterns and regional information, relating to the species and local climate, is useful in assessing their local significance. Adult Culicoides gnats are blood-sucking parasites and their bites are immediately painful and annoying for the horse. There is a characteristically rapid onset of pruritus, and the development of local papules and wheals at the site. Individual lesions last for several days, and frequent attacks cause almost continuous irritation. The majority of horses in a group are affected when the populations of Culicoides spp. are at their peak. In some enzootic areas in tropical and sub-tropical countries this can be continuous throughout the year. Culicoides spp. are most active at dusk and dawn, with little activity during the heat of the day and the cool of night. The preferred sites vary depending on the species, but the neck and back, the head, and ventral midline are commonly affected. They are also responsible for the development of a very common hypersensitivity disorder known as ‘sweet itch’ and for a ventral midline dermatitis.
"""
———————— TRY 2 (20250621)
<deepseek
"""
In Cuba, the term "jejenes" (also spelled "jején" in singular) refers to small biting midges or sand flies, primarily from two families:
1. Sand Flies (Psychodidae: Lutzomyia spp.)
- Most likely culprits for itchy, raised bites with a central dot.
- Tiny (1–3 mm), hairy, and weak fliers (often hop rather than fly).
- Active at dusk/dawn; bites can transmit leishmaniasis (rare but possible in rural Cuba).
- Microscope ID: Look for lance-shaped wings and a humpbacked appearance.
2. Biting Midges (Ceratopogonidae: Culicoides spp.)
- Called "jejenes" or "polvorines" in some regions.
- Even smaller (0.5–2 mm), with patterned wings.
- Bites are fiercely itchy and may bleed if scratched.
- Microscope ID: Check for spotted wings and short, stout mouthparts.Key Features Under the Microscope:
- Sand Flies:
- Humpbacked body, long legs, wings held erect like a "V."
- Larvae are aquatic/semi-aquatic (unlikely to see unless you sample soil/water).
- Biting Midges:
- Tiny, dark, with wing patterns (look for pigment spots).
- Larvae are in damp mud or rotting vegetation.
↓↓↓
Must be CULICOIDES !
———————— IDENTIFICATION
https://cjai.biologicalsurvey.ca/articles/jvlfcah-50/#keyEmbed
great resource
↓
[!!*o] Hard to identify, it is a real problem:
"""
Species level identification of Culicoides is difficult for a variety of reasons. Specimen collection is time-consuming and often requires specialized traps and/or equipment particular to each life stage. Observing such tiny organisms requires the use of high magnification, usually a microscope, to see even the most basic characteristics. Furthermore, specimens must also often be slide-mounted to observe diagnostic characters. Morphological identification of Culicoides often depends upon published species descriptions, which vary widely, and are often dated, cryptic, and based on subjective traits (Borkent and Grogan 2009). The identification process requires access to keys and descriptions from multiple sources (Swanson 2012), as well as a high degree of expertise in working with biting midges. The ability to identify Culicoides species is of increasing importance as the current climate crisis affects the distributions of several arthropod species of veterinary importance (Elbers et al. 2015; Vigil et al. 2018).
"""
https://www.mdpi.com/2075-4450/12/5/401
some photos
###
https://www.mdpi.com/2075-4450/12/4/366
nice photo of parts
https://bugguide.net/node/view/19768
###
¶Influenza (aka "flu")
https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal)
"""
There are 4 types of seasonal influenza viruses, types A, B, C and D. Influenza A and B viruses circulate and cause seasonal epidemics of disease.
"""
Influenza B is believed to be a milder virus compared to some strains of influenza A, such as H3N2, but more potent than the influenza A strains like H1N1 [4]. In fact, multiple studies have suggested increased potency of influenza B virus in causing severe disease and mortality.
"""
——————————— TREATMENT
treatment in complicated case with antivirals:
"""
oseltamivir = "tamiflu". prescription only, monitored.
----------------
https://medlineplus.gov/druginfo/meds/a699040.html
"""
There are four FDA-approved antiviral drugs recommended by CDC to treat flu this season.
https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal)
"""
There are 4 types of seasonal influenza viruses, types A, B, C and D. Influenza A and B viruses circulate and cause seasonal epidemics of disease.
- Influenza A viruses are further classified into subtypes according to the combinations of the hemagglutinin (HA) and the neuraminidase (NA), the proteins on the surface of the virus. Currently circulating in humans are subtype A(H1N1) and A(H3N2) influenza viruses. The A(H1N1) is also written as A(H1N1)pdm09 as it caused the pandemic in 2009 and subsequently replaced the seasonal influenza A(H1N1) virus which had circulated prior to 2009. Only influenza type A viruses are known to have caused pandemics.
- Influenza B viruses are not classified into subtypes, but can be broken down into lineages. Currently circulating influenza type B viruses belong to either B/Yamagata or B/Victoria lineage.
- Influenza C virus is detected less frequently and usually causes mild infections, thus does not present public health importance.
- Influenza D viruses primarily affect cattle and are not known to infect or cause illness in people.
"""
Influenza B is believed to be a milder virus compared to some strains of influenza A, such as H3N2, but more potent than the influenza A strains like H1N1 [4]. In fact, multiple studies have suggested increased potency of influenza B virus in causing severe disease and mortality.
"""
——————————— TREATMENT
treatment in complicated case with antivirals:
"""
- Neuraminidase inhibitors (i.e. oseltamivir) should be prescribed as soon as possible (ideally, within 48 hours following symptom onset) to maximize therapeutic benefits. Administration of the drug should also be considered in patients presenting later in the course of illness.
oseltamivir = "tamiflu". prescription only, monitored.
----------------
https://medlineplus.gov/druginfo/meds/a699040.html
"""
There are four FDA-approved antiviral drugs recommended by CDC to treat flu this season.
- oseltamivir phosphate (available as a generic version or under the trade name Tamiflu®),
- zanamivir (trade name Relenza®)
- peramivir (trade name Rapivab®), and.
- baloxavir marboxil (trade name Xofluza®).
¶[white rice→] Bacillus cereus
https://en.wikipedia.org/wiki/Rice#Bacillus_cereus
"""
Cooked rice can contain Bacillus cereus spores, which produce an emetic toxin when left at 4–60 °C (39–140 °F). When storing cooked rice for use the next day, rapid cooling is advised to reduce the risk of toxin production.[26] One of the enterotoxins produced by Bacillus cereus is heat-resistant; reheating contaminated rice kills the bacteria, but does not destroy the toxin already present.
"""
https://en.wikipedia.org/wiki/Bacillus_cereus
"""
Hours to multiply by 1,000,000 at 30°C:
Milk ~10h
Cooked rice ~9h
"""
GOD DAMN!
"""
is responsible for a minority of foodborne illnesses (2–5%), causing severe nausea, vomiting, and diarrhea.[39] Bacillus foodborne illnesses occur due to survival of the bacterial endospores when infected food is not, or is inadequately, cooked.[40] Cooking temperatures less than or equal to 100 °C (212 °F) allow some B. cereus spores to survive.[41] This problem is compounded when food is then improperly refrigerated, allowing the endospores to germinate.[
"""
"""
https://en.wikipedia.org/wiki/Rice#Bacillus_cereus
"""
Cooked rice can contain Bacillus cereus spores, which produce an emetic toxin when left at 4–60 °C (39–140 °F). When storing cooked rice for use the next day, rapid cooling is advised to reduce the risk of toxin production.[26] One of the enterotoxins produced by Bacillus cereus is heat-resistant; reheating contaminated rice kills the bacteria, but does not destroy the toxin already present.
"""
https://en.wikipedia.org/wiki/Bacillus_cereus
"""
Hours to multiply by 1,000,000 at 30°C:
Milk ~10h
Cooked rice ~9h
"""
GOD DAMN!
"""
is responsible for a minority of foodborne illnesses (2–5%), causing severe nausea, vomiting, and diarrhea.[39] Bacillus foodborne illnesses occur due to survival of the bacterial endospores when infected food is not, or is inadequately, cooked.[40] Cooking temperatures less than or equal to 100 °C (212 °F) allow some B. cereus spores to survive.[41] This problem is compounded when food is then improperly refrigerated, allowing the endospores to germinate.[
"""
"""
- The diarrheal type is associated with a wide range of foods, has an 8-to-16-hour incubation time, and is associated with diarrhea and gastrointestinal pain. Also known as the 'long-incubation' form of B. cereus food poisoning, it might be difficult to differentiate from poisoning caused by Clostridium perfringens.[45] Enterotoxin can be inactivated after heating at 56 °C (133 °F) for 5 minutes
- The 'emetic' form commonly results from rice which is cooked at a time and temperature insufficient to kill any spores present, then improperly refrigerated. The remaining spores can produce a toxin, cereulide, which is not inactivated by later reheating. This form leads to nausea and vomiting 1–5 hours after consumption. Distinguishing from other short-term bacterial foodborne intoxications, such as by Staphylococcus aureus, can be difficult.[45] Emetic toxin can withstand 121 °C (250 °F) for 90 minutes.[47]
¶(general Bacillus)
""
B. cereus and other members of Bacillus are not easily killed by alcohol; they have been known to colonize distilled liquors and alcohol-soaked swabs and pads in numbers sufficient to cause infection.[67][68]
"""
WTF
""
B. cereus and other members of Bacillus are not easily killed by alcohol; they have been known to colonize distilled liquors and alcohol-soaked swabs and pads in numbers sufficient to cause infection.[67][68]
"""
WTF
¶Wolbachia (bacteria infecting insects)
(now found in Cuba)
https://en.wikipedia.org/wiki/Wolbachia
"""
Wolbachia is a genus of intracellular bacteria that infects mainly arthropod species, including a high proportion of insects, and also some nematodes.[1][2] It is one of the most common parasitic microbes, and is possibly the most common reproductive parasite in the biosphere.[3] Its interactions with its hosts are often complex, and in some cases have evolved to be mutualistic rather than parasitic. Some host species cannot reproduce, or even survive, without Wolbachia colonisation. One study concluded that more than 16% of neotropical insect species carry bacteria of this genus,[4] and as many as 25 to 70% of all insect species are estimated to be potential hosts.[5
"""
Very weird:
* horizontal gene transfer agent
* because of quorum sensing, can be used actively as a counter some infections, like Zika)
* ###
(now found in Cuba)
https://en.wikipedia.org/wiki/Wolbachia
"""
Wolbachia is a genus of intracellular bacteria that infects mainly arthropod species, including a high proportion of insects, and also some nematodes.[1][2] It is one of the most common parasitic microbes, and is possibly the most common reproductive parasite in the biosphere.[3] Its interactions with its hosts are often complex, and in some cases have evolved to be mutualistic rather than parasitic. Some host species cannot reproduce, or even survive, without Wolbachia colonisation. One study concluded that more than 16% of neotropical insect species carry bacteria of this genus,[4] and as many as 25 to 70% of all insect species are estimated to be potential hosts.[5
"""
Very weird:
* horizontal gene transfer agent
* because of quorum sensing, can be used actively as a counter some infections, like Zika)
* ###
¶(dogs→) Cystic echinococcosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7971873/
"""
Cystic echinococcosis is one of the most important zoonotic diseases prevailing in different parts of Morocco [1, 2], as well as in other countries of North Africa and the Middle East [3]. Cystic echinococcosis is caused by the larval stage of the cestode Echinococcus granulosus [4] in humans as accidental hosts and a range of herbivores as natural intermediate hosts [5]. Dogs act as the definitive hosts and play an essential role in the dissemination of parasite eggs into the environment via their feces and contaminated fur [6–8]. In Morocco, areas with extensive sheep farming are severely affected since sheep are a very common intermediate host. The parasite’s cycle is poorly understood by the population, which severely affects compliance to the recommended hygiene measures aiming at reducing disease transmission [9]. Battelli [10] advocated for the integration of social, political and economic factors and argued for better use of available resources and adaptation of control strategies to the regional context.
"""
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7971873/
"""
Cystic echinococcosis is one of the most important zoonotic diseases prevailing in different parts of Morocco [1, 2], as well as in other countries of North Africa and the Middle East [3]. Cystic echinococcosis is caused by the larval stage of the cestode Echinococcus granulosus [4] in humans as accidental hosts and a range of herbivores as natural intermediate hosts [5]. Dogs act as the definitive hosts and play an essential role in the dissemination of parasite eggs into the environment via their feces and contaminated fur [6–8]. In Morocco, areas with extensive sheep farming are severely affected since sheep are a very common intermediate host. The parasite’s cycle is poorly understood by the population, which severely affects compliance to the recommended hygiene measures aiming at reducing disease transmission [9]. Battelli [10] advocated for the integration of social, political and economic factors and argued for better use of available resources and adaptation of control strategies to the regional context.
"""
¶(Mosquito→) Usutu virus
(found in Slo)
(SLO) https://nijz.si/nalezljive-bolezni/nalezljive-bolezni-od-a-do-z/usutu-virus-usuv/
"""
Usutu virus (USUV) is a flavivirus belonging to the Japanese encephalitis complex, which is an emerging zoonotic arbovirus of concern because of its pathogenicity to humans and its similarity in ecology with other emerging arboviruses such as West Nile virus.[1] It mainly infects Culex mosquitoes and birds; humans form a dead-end host. First identified in South Africa in 1959, the virus has caused outbreaks in birds across Europe since 1996. Nearly 50 cases in humans have been reported as of 2019, mainly in Europe. These are predominantly asymptomatic, but some people experience neurological symptoms.
"""
(found in Slo)
(SLO) https://nijz.si/nalezljive-bolezni/nalezljive-bolezni-od-a-do-z/usutu-virus-usuv/
"""
Usutu virus (USUV) is a flavivirus belonging to the Japanese encephalitis complex, which is an emerging zoonotic arbovirus of concern because of its pathogenicity to humans and its similarity in ecology with other emerging arboviruses such as West Nile virus.[1] It mainly infects Culex mosquitoes and birds; humans form a dead-end host. First identified in South Africa in 1959, the virus has caused outbreaks in birds across Europe since 1996. Nearly 50 cases in humans have been reported as of 2019, mainly in Europe. These are predominantly asymptomatic, but some people experience neurological symptoms.
"""
¶(Mosquito→) Sindbis virus
(found in Slo)
https://en.wikipedia.org/wiki/Sindbis_virus
"""
Sindbis virus (SINV) is a member of the Togaviridae family, in the Alphavirus genus. The virus was first isolated in 1952 in Cairo, Egypt.[2] The virus is transmitted by mosquitoes (Culex and Culiseta). SINV is linked to Pogosta disease[3] (Finland), Ockelbo disease (Sweden) and Karelian fever (Russia). In humans, the symptoms include arthralgia, rash and malaise. Sindbis virus is widely and continuously found in insects and vertebrates in Eurasia, Africa, and Oceania. Clinical infection and disease in humans however has almost only been reported from Northern Europe (Finland, Sweden, Russian Karelia), where SINV is endemic and where large outbreaks occur intermittently. Cases are occasionally reported in Australia, China, and South Africa.[4]
SINV is an arbovirus, it is arthropod-borne, and it is maintained in nature by transmission between vertebrate (bird) hosts and invertebrate (mosquito) vectors. Humans are infected with Sindbis virus when bitten by an infected mosquito.
"""
(found in Slo)
https://en.wikipedia.org/wiki/Sindbis_virus
"""
Sindbis virus (SINV) is a member of the Togaviridae family, in the Alphavirus genus. The virus was first isolated in 1952 in Cairo, Egypt.[2] The virus is transmitted by mosquitoes (Culex and Culiseta). SINV is linked to Pogosta disease[3] (Finland), Ockelbo disease (Sweden) and Karelian fever (Russia). In humans, the symptoms include arthralgia, rash and malaise. Sindbis virus is widely and continuously found in insects and vertebrates in Eurasia, Africa, and Oceania. Clinical infection and disease in humans however has almost only been reported from Northern Europe (Finland, Sweden, Russian Karelia), where SINV is endemic and where large outbreaks occur intermittently. Cases are occasionally reported in Australia, China, and South Africa.[4]
SINV is an arbovirus, it is arthropod-borne, and it is maintained in nature by transmission between vertebrate (bird) hosts and invertebrate (mosquito) vectors. Humans are infected with Sindbis virus when bitten by an infected mosquito.
"""
¶Vibrio vulnificus
https://en.wikipedia.org/wiki/Vibrio_vulnificus
"""
Present in marine environments such as estuaries, brackish ponds, or coastal areas, V. vulnificus is related to V. cholerae, the causative agent of cholera.[3][4] At least one strain of V. vulnificus is bioluminescent.[5]
"""
-------------------
"""
Vibrio vulnificus is an extremely virulent bacterium that can cause three types of infections:
"""
------------------------
Needs iron
"""
Iron: Growth of V. vulnificus is dependent on the amount of iron that is accessible to the bacteria.[18][19][20] The observed association of the infection with liver disease (associated with increased serum iron) might be due to the capability of more virulent strains to capture iron bound to transferrin.[12]
"""
https://en.wikipedia.org/wiki/Vibrio_vulnificus
"""
Present in marine environments such as estuaries, brackish ponds, or coastal areas, V. vulnificus is related to V. cholerae, the causative agent of cholera.[3][4] At least one strain of V. vulnificus is bioluminescent.[5]
"""
-------------------
"""
Vibrio vulnificus is an extremely virulent bacterium that can cause three types of infections:
- Acute gastroenteritis from eating raw or undercooked shellfish: V. vulnificus causes an infection often incurred after eating seafood, especially raw or undercooked oysters. It does not alter the appearance, taste, or odor of oysters.[8] Symptoms include vomiting, diarrhea, and abdominal pain.
- Necrotizing wound infections can occur in injured skin exposed to contaminated marine water. V. vulnificus bacteria can enter the body through open wounds when swimming or wading in infected waters,[4] or by puncture wounds from the spines of fishes such as stingrays. People may develop a blistering dermatitis sometimes mistaken for pemphigus or pemphigoid.
- Invasive sepsis can occur after eating raw or undercooked shellfish, especially oysters. V. vulnificus is 80 times more likely to spread into the bloodstream in people with compromised immune systems, especially those with chronic liver disease. When this happens, severe symptoms including blistering skin lesions and septic shock can sometimes lead to death.[9][10] This severe infection may occur regardless of whether the infection began from contaminated food or an open wound.[10]
"""
------------------------
Needs iron
"""
Iron: Growth of V. vulnificus is dependent on the amount of iron that is accessible to the bacteria.[18][19][20] The observed association of the infection with liver disease (associated with increased serum iron) might be due to the capability of more virulent strains to capture iron bound to transferrin.[12]
"""
¶FUNGAL— Infectious fungal spores (for lungs)
Case of "bad cigar"
<gpt
"""
If cigars were contaminated with fungal spores, and you smoked them, there would be a potential risk of inhaling those spores. Inhaling fungal spores can lead to various respiratory issues, depending on the type of fungus involved and the individual's immune system. Some fungi can cause lung infections, including:
* Aspergillosis: Aspergillus is a common fungus that can be found in the environment. Inhaling its spores can lead to aspergillosis, which can manifest as allergic bronchopulmonary aspergillosis (ABPA), chronic pulmonary aspergillosis (CPA), or invasive pulmonary aspergillosis (IPA), with varying degrees of severity.
* Hypersensitivity Pneumonitis: Some people may develop hypersensitivity pneumonitis when exposed to certain fungal spores, particularly in occupational or environmental settings. This condition is an inflammatory lung disease that can result from repeated exposure to organic dust, including fungal spores.
* Fungal Lung Infections: Inhaling certain fungal spores, especially in individuals with weakened immune systems, can lead to fungal lung infections. These infections can be serious and may require medical treatment.
It's important to note that the presence of fungal spores in a cigar would be highly unusual and is not a common concern associated with smoking cigars. Cigars are typically made from tobacco leaves, and fungal contamination is not a typical issue during their production. However, if you have reason to believe that a cigar or any tobacco product has been exposed to mold or fungal contamination, it's best to avoid using it to reduce the risk of potential health problems.
In general, if you experience respiratory symptoms or have concerns about your lung health after inhaling or being exposed to potentially contaminated substances, it's advisable to seek medical attention for a proper evaluation and guidance on treatment if necessary.
"""
Case of "bad cigar"
<gpt
"""
If cigars were contaminated with fungal spores, and you smoked them, there would be a potential risk of inhaling those spores. Inhaling fungal spores can lead to various respiratory issues, depending on the type of fungus involved and the individual's immune system. Some fungi can cause lung infections, including:
* Aspergillosis: Aspergillus is a common fungus that can be found in the environment. Inhaling its spores can lead to aspergillosis, which can manifest as allergic bronchopulmonary aspergillosis (ABPA), chronic pulmonary aspergillosis (CPA), or invasive pulmonary aspergillosis (IPA), with varying degrees of severity.
* Hypersensitivity Pneumonitis: Some people may develop hypersensitivity pneumonitis when exposed to certain fungal spores, particularly in occupational or environmental settings. This condition is an inflammatory lung disease that can result from repeated exposure to organic dust, including fungal spores.
* Fungal Lung Infections: Inhaling certain fungal spores, especially in individuals with weakened immune systems, can lead to fungal lung infections. These infections can be serious and may require medical treatment.
It's important to note that the presence of fungal spores in a cigar would be highly unusual and is not a common concern associated with smoking cigars. Cigars are typically made from tobacco leaves, and fungal contamination is not a typical issue during their production. However, if you have reason to believe that a cigar or any tobacco product has been exposed to mold or fungal contamination, it's best to avoid using it to reduce the risk of potential health problems.
In general, if you experience respiratory symptoms or have concerns about your lung health after inhaling or being exposed to potentially contaminated substances, it's advisable to seek medical attention for a proper evaluation and guidance on treatment if necessary.
"""
¶(pneumonia causing)
"""
Kaj vsebuje zdravilo Broncho-Munal
Učinkovina je lizat bakterij, ki najpogosteje povzročajo okužbe dihal:
Diplococcus pneumoniae,
Haemophilus influenzae,
Klebsiella pneumoniae,
Klebsiella ozaenae,
Staphylococcus aureus,
Streptococcus viridans,
Streptococcus pyogenes,
Neisseria catarrhalis.
"""
"""
Diplococcus pneumoniae,
Haemophilus influenzae,
Klebsiella pneumoniae,
Klebsiella ozaenae,
Staphylococcus aureus,
Streptococcus viridans,
Streptococcus pyogenes,
Neisseria catarrhalis.
"""
¶Clostridium
long-threat
"""
Clostridium difficile (C. diff): The spores of C. difficile, a bacterium responsible for gastrointestinal infections, can survive on surfaces for extended periods and are resistant to many disinfectants.
"""
long-threat
"""
Clostridium difficile (C. diff): The spores of C. difficile, a bacterium responsible for gastrointestinal infections, can survive on surfaces for extended periods and are resistant to many disinfectants.
"""
¶Hepatitis C
https://www.hiv.gov/blog/scientists-discover-hepatitis-c-virus-can-remain-infectious-outside-of-the-body-for-up-to-6-weeks/
(!)
https://www.hiv.gov/blog/scientists-discover-hepatitis-c-virus-can-remain-infectious-outside-of-the-body-for-up-to-6-weeks/
(!)
¶(cats/###→) Bartonella → Bartonellosis
<bard
"""
Bartonellosis is a group of bacterial infections that can be transmitted to humans from animals, mainly cats. There are over 20 species of Bartonella bacteria, but three are the most common causes of human infection in Europe:
The symptoms of bartonellosis can vary depending on the species of bacterium that is responsible for the infection. However, some of the most common symptoms include:
In some cases, bartonellosis can cause more serious complications, such as:
If you are concerned that you may have bartonellosis, it is important to see a doctor. The doctor will likely do a physical examination and ask you about your symptoms. They may also order blood tests to check for the presence of bartonellosis antibodies.
Bartonellosis is usually treated with antibiotics. The type of antibiotic and the length of treatment will depend on the species of bacterium causing the infection and the severity of the symptoms.
In conclusion, bartonellosis is a group of bacterial infections that can be transmitted to humans from animals, mainly cats. It is a relatively common infection in Europe, with an estimated prevalence of between 1% and 5% of the population. The symptoms of bartonellosis can vary depending on the species of bacterium that is responsible for the infection, but some of the most common symptoms include fever, flu-like symptoms, swollen lymph nodes, and skin lesions. In some cases, bartonellosis can cause more serious complications, such as cat scratch disease, bacillary angiomatosis, and Carrion's disease. If you are concerned that you may have bartonellosis, it is important to see a doctor.
""
<bard
"""
Bartonellosis is a group of bacterial infections that can be transmitted to humans from animals, mainly cats. There are over 20 species of Bartonella bacteria, but three are the most common causes of human infection in Europe:
- Bartonella henselae: This is the most common cause of bartonellosis in Europe. It is usually transmitted by cat fleas, but can also be transmitted through cat bites or scratches.
- Bartonella quintana: This bacterium is responsible for trench fever, a disease that was common in soldiers during World War I. It is transmitted by human body lice.
- Bartonella bacilliformis: This bacterium is responsible for Oroya fever, a serious disease that is endemic to the Andes Mountains in South America. It is transmitted by sandflies.
The symptoms of bartonellosis can vary depending on the species of bacterium that is responsible for the infection. However, some of the most common symptoms include:
- Fever
- Flu-like symptoms, such as fatigue, muscle aches, and headache
- Swollen lymph nodes
- Skin lesions, such as red bumps or ulcers
In some cases, bartonellosis can cause more serious complications, such as:
- Cat scratch disease: This is a common infection in children. It is usually caused by Bartonella henselae and is characterized by a small, red bump at the site of the scratch. The person may also experience fever, headache, and swollen lymph nodes.
- Bacilloid angiomatosis: This is a rare condition that is characterized by the growth of blood vessels in the skin and other organs. It can be caused by Bartonella henselae or Bartonella quintana.
- Carrion's disease: This is a severe infection that is caused by Bartonella bacilliformis. It is endemic to the Andes Mountains in South America and is characterized by fever, chills, muscle aches, headache, and skin lesions.
If you are concerned that you may have bartonellosis, it is important to see a doctor. The doctor will likely do a physical examination and ask you about your symptoms. They may also order blood tests to check for the presence of bartonellosis antibodies.
Bartonellosis is usually treated with antibiotics. The type of antibiotic and the length of treatment will depend on the species of bacterium causing the infection and the severity of the symptoms.
In conclusion, bartonellosis is a group of bacterial infections that can be transmitted to humans from animals, mainly cats. It is a relatively common infection in Europe, with an estimated prevalence of between 1% and 5% of the population. The symptoms of bartonellosis can vary depending on the species of bacterium that is responsible for the infection, but some of the most common symptoms include fever, flu-like symptoms, swollen lymph nodes, and skin lesions. In some cases, bartonellosis can cause more serious complications, such as cat scratch disease, bacillary angiomatosis, and Carrion's disease. If you are concerned that you may have bartonellosis, it is important to see a doctor.
""
¶(pigeon shit→) fungal spores → fungal pneumonias, ...
<chatgpt
"""
Here's a table outlining the typical incubation periods for some common diseases associated with exposure to pigeon droppings:
Histoplasmosis Histoplasma capsulatum 3-17 days
Cryptococcosis Cryptococcus neoformans 2-12 weeks
### another source casy 2-13 months!
### "Individual case incubation periods ranged from 2 to 11 months, with a median of 6 to 7 months"
Psittacosis Chlamydia psittaci 5-14 days
Salmonellosis Salmonella bacteria 6-72 hours
E. coli Infection Escherichia coli bacteria 1-10 days
Ectoparasite-related diseases Various ectoparasites Varies depending on specific parasite and individual response
Respiratory Irritations Allergens and irritants in droppings Immediate to several days
"""
https://www.ncbi.nlm.nih.gov/books/NBK431060/
(general info)
"""
Cryptococcus neoformans and Cryptococcus gatti both spread through inhalation and cause a similar spectrum of illness. Despite lung being the common site where the pathogen enters the body meningoencephalitis is the most common clinical manifestation of the infection. Clinical features of cryptococcal meningitis typically manifest with in 1-2 weeks and include fever, malaise, headache, neck stiffness, photophobia, nausea, and vomiting.
"""
(shorter??)
https://www.uptodate.com/contents/cryptococcus-gattii-infection-clinical-features-and-diagnosis/print
The proportion of C. gattii disease representing acute infection versus reactivation of latent infection remains unknown; however, most reported cases of C. gattii infection appear to be primary infections.
https://www.cdc.gov/fungal/diseases/cryptococcosis-gattii/symptoms.html
"""
The incubation period of C. gattii infection is not well-established.
Symptoms of C. gattii infection can appear between two and 13 months after breathing in the fungus, with an average of approximately six to seven months.
However, people can develop an infection as soon as two weeks or as late as three years after breathing in the fungus
"""
_______ DIAGNOSIS/TESTING
<chatgpt
"""
The time it takes for a blood test to detect Cryptococcus neoformans antigens or antibodies after inhalation can vary.
However, in cases of acute infection, these antigens or antibodies may be detectable within days to weeks after exposure.
Specifically, blood tests such as cryptococcal antigen testing (often performed using a serum sample) can detect cryptococcal antigens relatively quickly. This test looks for the presence of cryptococcal polysaccharide antigens in the bloodstream, which are released by Cryptococcus neoformans during infection. In some cases, antigenemia (presence of antigens in the blood) may be detectable within a few days to a couple of weeks after exposure, depending on factors such as the individual's immune response and the severity of the infection.
"""
https://www.publichealthontario.ca/en/Laboratory-Services/Test-Information-Index/Cryptococcus-Direct-Blood-CSF
<chatgpt
"""
Here's a table outlining the typical incubation periods for some common diseases associated with exposure to pigeon droppings:
Histoplasmosis Histoplasma capsulatum 3-17 days
Cryptococcosis Cryptococcus neoformans 2-12 weeks
### another source casy 2-13 months!
### "Individual case incubation periods ranged from 2 to 11 months, with a median of 6 to 7 months"
Psittacosis Chlamydia psittaci 5-14 days
Salmonellosis Salmonella bacteria 6-72 hours
E. coli Infection Escherichia coli bacteria 1-10 days
Ectoparasite-related diseases Various ectoparasites Varies depending on specific parasite and individual response
Respiratory Irritations Allergens and irritants in droppings Immediate to several days
"""
https://www.ncbi.nlm.nih.gov/books/NBK431060/
(general info)
"""
Cryptococcus neoformans and Cryptococcus gatti both spread through inhalation and cause a similar spectrum of illness. Despite lung being the common site where the pathogen enters the body meningoencephalitis is the most common clinical manifestation of the infection. Clinical features of cryptococcal meningitis typically manifest with in 1-2 weeks and include fever, malaise, headache, neck stiffness, photophobia, nausea, and vomiting.
"""
(shorter??)
https://www.uptodate.com/contents/cryptococcus-gattii-infection-clinical-features-and-diagnosis/print
The proportion of C. gattii disease representing acute infection versus reactivation of latent infection remains unknown; however, most reported cases of C. gattii infection appear to be primary infections.
https://www.cdc.gov/fungal/diseases/cryptococcosis-gattii/symptoms.html
"""
The incubation period of C. gattii infection is not well-established.
Symptoms of C. gattii infection can appear between two and 13 months after breathing in the fungus, with an average of approximately six to seven months.
However, people can develop an infection as soon as two weeks or as late as three years after breathing in the fungus
"""
_______ DIAGNOSIS/TESTING
<chatgpt
"""
The time it takes for a blood test to detect Cryptococcus neoformans antigens or antibodies after inhalation can vary.
However, in cases of acute infection, these antigens or antibodies may be detectable within days to weeks after exposure.
Specifically, blood tests such as cryptococcal antigen testing (often performed using a serum sample) can detect cryptococcal antigens relatively quickly. This test looks for the presence of cryptococcal polysaccharide antigens in the bloodstream, which are released by Cryptococcus neoformans during infection. In some cases, antigenemia (presence of antigens in the blood) may be detectable within a few days to a couple of weeks after exposure, depending on factors such as the individual's immune response and the severity of the infection.
"""
https://www.publichealthontario.ca/en/Laboratory-Services/Test-Information-Index/Cryptococcus-Direct-Blood-CSF
¶(...→) Psitaccosis
aka Psittacosis Chlamydiosis, Ornithosis, Parrot Fever
https://www.nj.gov/agriculture/divisions/ah/diseases/psittacosis.html
"""
In birds, chlamydiosis results from infection by Chlamydophila psittaci (order Chlamydiales, family Chlamydiaceae). This organism, previously known as Chlamydia psittaci, is a Gram negative, coccoid, obligate intracellular bacterium. There are at least six avian serotypes.
Geographic Distribution
Avian chlamydiosis can be found worldwide. C. psittaci is particularly common in psittacine birds in tropical and subtropical regions. This disease is present in the United States. In a 1982 survey, C. psittaci was isolated from 20-50% of necropsied pet birds in California and Florida.
[...]
The incubation period in humans is 1 to 4 weeks; most infections become symptomatic after 10 days.
"""
aka Psittacosis Chlamydiosis, Ornithosis, Parrot Fever
https://www.nj.gov/agriculture/divisions/ah/diseases/psittacosis.html
"""
In birds, chlamydiosis results from infection by Chlamydophila psittaci (order Chlamydiales, family Chlamydiaceae). This organism, previously known as Chlamydia psittaci, is a Gram negative, coccoid, obligate intracellular bacterium. There are at least six avian serotypes.
Geographic Distribution
Avian chlamydiosis can be found worldwide. C. psittaci is particularly common in psittacine birds in tropical and subtropical regions. This disease is present in the United States. In a 1982 survey, C. psittaci was isolated from 20-50% of necropsied pet birds in California and Florida.
[...]
The incubation period in humans is 1 to 4 weeks; most infections become symptomatic after 10 days.
"""
¶Listeria monocytogenes
https://www.celjske-mesnine.si/obvestilo/odpoklic-sunka-sendvic/ (20240717)
"""
Razlogi neustreznosti: potrošnike obveščamo, da je bila v živilu ugotovljena prisotnost bakterije Listeria Razlogi neustreznosti: potrošnike obveščamo, da je bila v živilu ugotovljena prisotnost bakterije Listeria monocytogenes, ki lahko pri potrošnikih povzroči črevesne težave (driska, bruhanje,... ) ali simptome gripe/prehlada. V primeru ugotovljenih zdravstvenih težav se nemudoma obrnite na svojega zdravnika ali na epidemiologa regionalnega zavoda za zdravstveno varstvo., ki lahko pri potrošnikih povzroči črevesne težave (driska, bruhanje,... ) ali simptome gripe/prehlada. V primeru ugotovljenih zdravstvenih težav se nemudoma obrnite na svojega zdravnika ali na epidemiologa regionalnega zavoda za zdravstveno varstvo.
"""
https://www.celjske-mesnine.si/obvestilo/odpoklic-sunka-sendvic/ (20240717)
"""
Razlogi neustreznosti: potrošnike obveščamo, da je bila v živilu ugotovljena prisotnost bakterije Listeria Razlogi neustreznosti: potrošnike obveščamo, da je bila v živilu ugotovljena prisotnost bakterije Listeria monocytogenes, ki lahko pri potrošnikih povzroči črevesne težave (driska, bruhanje,... ) ali simptome gripe/prehlada. V primeru ugotovljenih zdravstvenih težav se nemudoma obrnite na svojega zdravnika ali na epidemiologa regionalnega zavoda za zdravstveno varstvo., ki lahko pri potrošnikih povzroči črevesne težave (driska, bruhanje,... ) ali simptome gripe/prehlada. V primeru ugotovljenih zdravstvenih težav se nemudoma obrnite na svojega zdravnika ali na epidemiologa regionalnega zavoda za zdravstveno varstvo.
"""
¶TICKS— Ticks → Francisella tularensis → Tularemia
slo: "zajčja mrzlica"
2024: https://www.gorenjskiglas.si/article/20240730/C/240739998/1169/zajcja-mrzlica--uporabite-masko-ffp3
manifests as pneumonia, but needs different AB
"""
Tularemijo prenašajo predvsem zajci in okuženi klopi, pa tudi muhe, bolhe, uši in komarji. Okužba je možna tudi z vdihavanjem okuženega prahu, uživanjem premalo toplotno obdelanih živil in okužene vode. Kot poudarjajo na Kliniki Golnik, se simptomi razlikujejo glede na vstopno mesto bakterije v telo. Pri vstopu prek vboda klopa ali pika komarja se na mestu vboda pojavi razjeda. Zaužitje bakterije z neprekuhanim mlekom okuženih živali lahko povzroči prebavne težave, vdihavanje bakterije pa hudo obliko pljučnice. Opozarjajo, da se bolezen ne prenaša s človeka na človeka in običajno nastopi od tri do šest dni po okužbi.
"""
via mosquito/fly/tick → ulcerated sore (lesion) at bite site
slo: "zajčja mrzlica"
2024: https://www.gorenjskiglas.si/article/20240730/C/240739998/1169/zajcja-mrzlica--uporabite-masko-ffp3
manifests as pneumonia, but needs different AB
"""
Tularemijo prenašajo predvsem zajci in okuženi klopi, pa tudi muhe, bolhe, uši in komarji. Okužba je možna tudi z vdihavanjem okuženega prahu, uživanjem premalo toplotno obdelanih živil in okužene vode. Kot poudarjajo na Kliniki Golnik, se simptomi razlikujejo glede na vstopno mesto bakterije v telo. Pri vstopu prek vboda klopa ali pika komarja se na mestu vboda pojavi razjeda. Zaužitje bakterije z neprekuhanim mlekom okuženih živali lahko povzroči prebavne težave, vdihavanje bakterije pa hudo obliko pljučnice. Opozarjajo, da se bolezen ne prenaša s človeka na človeka in običajno nastopi od tri do šest dni po okužbi.
"""
via mosquito/fly/tick → ulcerated sore (lesion) at bite site
¶(flies) → myiasis
https://en.wikipedia.org/wiki/Myiasis
"""
Myiasis (/maɪ.ˈaɪ.ə.səs/ my-EYE-ə-səss[1]), also known as flystrike or fly strike, is the parasitic infestation of the body of a live animal by fly larvae (maggots) that grow inside the host while feeding on its tissue. Although flies are most commonly attracted to open wounds and urine- or feces-soaked fur, some species (including the most common myiatic flies—the botfly, blowfly, and screwfly) can create an infestation even on unbroken skin and have been known to use moist soil and non-myiatic flies (such as the common housefly) as vector agents for their parasitic larvae.
"""
all common flies:
including "black" housefly, "green" blowfly, etc
https://en.wikipedia.org/wiki/Psychodidae
<----------------------- (NEW)+ UNSORTED HORROR ↑
https://en.wikipedia.org/wiki/Myiasis
"""
Myiasis (/maɪ.ˈaɪ.ə.səs/ my-EYE-ə-səss[1]), also known as flystrike or fly strike, is the parasitic infestation of the body of a live animal by fly larvae (maggots) that grow inside the host while feeding on its tissue. Although flies are most commonly attracted to open wounds and urine- or feces-soaked fur, some species (including the most common myiatic flies—the botfly, blowfly, and screwfly) can create an infestation even on unbroken skin and have been known to use moist soil and non-myiatic flies (such as the common housefly) as vector agents for their parasitic larvae.
"""
all common flies:
including "black" housefly, "green" blowfly, etc
https://en.wikipedia.org/wiki/Psychodidae
<----------------------- (NEW)+ UNSORTED HORROR ↑
¶PRACTICAL QUESTIONS [!!]
* I have a few flea bites in ankles, omg what to do now ?
* How easy is it to get bedbugs if you don't sleep / sit down on textile in a home that's infested ?
* How to positively ID bedbugs vs fleas?
* Will cat/dog fleas only "bit a few times", or will they go and spread?:
and, if you remove the cat from the apartment, are they really going to go on you? (and keep going?)
* What of these can you get from pets?:
* Scabies: not really (different type)
* [...]
<------------------- (new) basic questions ↑
* I have a few flea bites in ankles, omg what to do now ?
* How easy is it to get bedbugs if you don't sleep / sit down on textile in a home that's infested ?
* How to positively ID bedbugs vs fleas?
* Will cat/dog fleas only "bit a few times", or will they go and spread?:
and, if you remove the cat from the apartment, are they really going to go on you? (and keep going?)
* What of these can you get from pets?:
* Scabies: not really (different type)
* [...]
<------------------- (new) basic questions ↑
¶BASIC TIPS !
These need checks [!!]
* keeping clothes:
* separate clothes well (dirty / in use / clean)
* keep clothes in well-sealed bags and don't let any shit out:
< photo > .. also establish it's good enough?
* [...]
* use Fenistil?:
seems no side effects
* [...]
These need checks [!!]
* keeping clothes:
* separate clothes well (dirty / in use / clean)
* keep clothes in well-sealed bags and don't let any shit out:
* [...]
* use Fenistil?:
seems no side effects
* [...]
¶Prevention !
* do polyester covers help ???
* wearing specific clothes ("long socks, etc") ?
* how to evade pet contact? just don't let them rub on you eh?
* seems all of them generally hate some natural things (tea trea oil, lavender, etc)
* do polyester covers help ???
* wearing specific clothes ("long socks, etc") ?
* how to evade pet contact? just don't let them rub on you eh?
* seems all of them generally hate some natural things (tea trea oil, lavender, etc)
¶Identification online
:
* https://www.facebook.com/groups/Insect.Identification/
* https://bugguide.net
* https://www.nhm.ac.uk/natureplus/community/identification/bug-forum@view=overview.html
* https://garden.org/forums/view/otherid/
* [...]
:
* https://www.facebook.com/groups/Insect.Identification/
* https://bugguide.net
* https://www.nhm.ac.uk/natureplus/community/identification/bug-forum@view=overview.html
* https://garden.org/forums/view/otherid/
* [...]
¶Identification (by eye & microscope)
http://www.howtogetridofgnat.com/2014/11/how-to-identify-biting-gnats-and-noseeums-with-pictures-of-biting-flies-and-non-biting-flies.html
not the best but some ideas
doesn't include many important species
___________
Very nice for larval types:
https://entomology.ca.uky.edu/ef017
(more a nice example of a guide, than useful in this case)
http://www.howtogetridofgnat.com/2014/11/how-to-identify-biting-gnats-and-noseeums-with-pictures-of-biting-flies-and-non-biting-flies.html
not the best but some ideas
doesn't include many important species
___________
Very nice for larval types:
https://entomology.ca.uky.edu/ef017
(more a nice example of a guide, than useful in this case)
¶Handbook for identification of fruitflies
* description for how to pin them!
* very good photographic doc, comparing different types!
https://www.planthealthaustralia.com.au/wp-content/uploads/2018/10/The-Australian-Handbook-for-the-Identification-of-Fruit-Flies-v3.1.pdf
* description for how to pin them!
* very good photographic doc, comparing different types!
https://www.planthealthaustralia.com.au/wp-content/uploads/2018/10/The-Australian-Handbook-for-the-Identification-of-Fruit-Flies-v3.1.pdf
¶Trap: smaller flies (including punkies)
with vinegar+soap
https://www.charlestoncitypaper.com/charleston/how-to-rid-your-house-of-no-see-ums/Content?oid=3671085
with vinegar+soap
https://www.charlestoncitypaper.com/charleston/how-to-rid-your-house-of-no-see-ums/Content?oid=3671085
¶Using salt?
Salt is abundand in Canaries... so can you use it as antipest?
YES and NO:
* It is repellent and potentially prevents you from having roaches
* BUT it does NOT KILL them
--> """ ... it’s not really meant for major pest control. However, it’s still worth a try though. After all, it’s one of the most inexpensive alternatives to pesticides."""
https://fightbugs.com/roaches-attracted-to-salt/
What to do:
* """All you have to do is sprinkle the condiment onto roach infested areas to keep them from coming back. Toss salt on your toolshed, car, basement and attic to stop those insects from nesting there. You can also sprinkle the condiment all over your kitchen, so your food won’t get contaminated by roaches."""
https://fightbugs.com/roaches-attracted-to-salt/
Salt is abundand in Canaries... so can you use it as antipest?
YES and NO:
* It is repellent and potentially prevents you from having roaches
* BUT it does NOT KILL them
--> """ ... it’s not really meant for major pest control. However, it’s still worth a try though. After all, it’s one of the most inexpensive alternatives to pesticides."""
https://fightbugs.com/roaches-attracted-to-salt/
What to do:
* """All you have to do is sprinkle the condiment onto roach infested areas to keep them from coming back. Toss salt on your toolshed, car, basement and attic to stop those insects from nesting there. You can also sprinkle the condiment all over your kitchen, so your food won’t get contaminated by roaches."""
https://fightbugs.com/roaches-attracted-to-salt/
¶[!*!→] MEDICAL— Rehydration (common for viral diseases)
"""
Fruit juices both provide water and electrolytes, and contain many essential vitamins and minerals, help strengthen the immune system, increase the stability of the vessel walls, thereby reducing the risk of bleeding; Filtered water: Dengue patients need to rehydrate enough in the treatment of dengue fever, focus on ...
"""
https://www.herminahospitals.com/en/articles/5-minuman-yang-dapat-atasi-gejala-demam-berdarah-dengue-dbd
<------------------------- (new) ACTION! ↑
"""
Fruit juices both provide water and electrolytes, and contain many essential vitamins and minerals, help strengthen the immune system, increase the stability of the vessel walls, thereby reducing the risk of bleeding; Filtered water: Dengue patients need to rehydrate enough in the treatment of dengue fever, focus on ...
"""
https://www.herminahospitals.com/en/articles/5-minuman-yang-dapat-atasi-gejala-demam-berdarah-dengue-dbd
<------------------------- (new) ACTION! ↑
¶[!] How do hotels prevent bedbugs (etc) ???
"""
Bed bug infestations in hotel rooms are are actually easier to eradicate in most cases. The rooms are not cluttered with clothes and personal belongings. You only have the structure and furniture. Once bed bugs are discovered, the rooms are treated in the same manner as one would treat a residential infestation. The process is just easier.
"""
Important for #reconf !
"""
Bed bug infestations in hotel rooms are are actually easier to eradicate in most cases. The rooms are not cluttered with clothes and personal belongings. You only have the structure and furniture. Once bed bugs are discovered, the rooms are treated in the same manner as one would treat a residential infestation. The process is just easier.
"""
Important for #reconf !
¶Eradication by genetic-modified sterilized males, etc
https://en.wikipedia.org/wiki/Aedes_aegypti#Genetic_modification
https://www.popsci.com/spanish-drone-will-drop-insects-over-ethiopia-to-fight-disease/
https://en.wikipedia.org/wiki/Aedes_aegypti#Genetic_modification
https://www.popsci.com/spanish-drone-will-drop-insects-over-ethiopia-to-fight-disease/
¶[!!] Get a ultraviolet light
@@ordering
"""Secondly an ultra violet certainly allows for better detection of bed bugs but a normal bright LED flashlight is a huge help as well"""
OR NOT ?
"""Contrary to what you may have read elsewhere an ultra-violet light does not make it easier to spot bedbugs. I have personally verified this!"""
OR ...
https://citypests.com/uv-light-detect-and-kill-bed-bugs/
______________
#tobuy
BLACK LIGHT FLASHLIGHT:
What's the right light nm?
@@ordering
* ~395nm (was sold somewhere)
* wood lamp ~365nm ?
"""Woodova svetilka je ultravijolična svetilka s steklenim filtrom, ki prepušča le UV svetlobo z valovno dolžino 365 nm."""
@@ordering
"""Secondly an ultra violet certainly allows for better detection of bed bugs but a normal bright LED flashlight is a huge help as well"""
OR NOT ?
"""Contrary to what you may have read elsewhere an ultra-violet light does not make it easier to spot bedbugs. I have personally verified this!"""
OR ...
https://citypests.com/uv-light-detect-and-kill-bed-bugs/
______________
#tobuy
BLACK LIGHT FLASHLIGHT:
What's the right light nm?
* ~395nm (was sold somewhere)
* wood lamp ~365nm ?
¶Raising Cockroaches Intentionally
Check this tutorial : https://www.instructables.com/id/Raising-Cockroaches-Intentionally/
<---------------------------------- ### (NOW) REVIEWING
Check this tutorial : https://www.instructables.com/id/Raising-Cockroaches-Intentionally/
<---------------------------------- ### (NOW) REVIEWING
¶REPRESENTATION SYSTEMS -- Ecosystem/ecotype/bio-connectomes
#TODO !!!
Are they too big to show, again?
#TODO !!!
Are they too big to show, again?
¶Research more on "natural enemies"
:
* what is in currently in use?
* any finished success stories?
* what went wrong in past? what is said that could go wrong?
* what are novel/suggested approaches?
__________
* what would be the smallest scale this could be done?
review !!!:
* https://faculty.ucr.edu/~legneref/biotact/detailed.htm
* [...]
:
* what is in currently in use?
* any finished success stories?
* what went wrong in past? what is said that could go wrong?
* what are novel/suggested approaches?
__________
* what would be the smallest scale this could be done?
review !!!:
* https://faculty.ucr.edu/~legneref/biotact/detailed.htm
* [...]
¶Evania appendigaster: Anti-cockroaches wasp
https://en.wikipedia.org/wiki/Evania_appendigaster
"""
Evania appendigaster is a species of wasp in the family Evaniidae, the ensign wasps. Its native range is not known, but it likely originated in Asia. Today it occurs throughout the tropics and subtropics and in many temperate regions. It is a parasitoid wasp known for specializing on cockroaches.[1]
[...]
The wasp may be a candidate for use as an agent of biological pest control of cockroaches.[5][8] Control might be even better if the wasp were released along with A. hagenowii, which tends to have a higher rate of parasitism.[1]
"""
________________
another one!
https://en.wikipedia.org/wiki/Emerald_cockroach_wasp
"Ampulex compressa"
great:
* https://www.youtube.com/watch?v=ovo_T0KqdYg
* https://www.youtube.com/watch?v=-ySwuQhruBo
* [...]
________________
More on both species as "NATURAL ENEMIES":
* https://faculty.ucr.edu/~legneref/biotact/ch-27.htm
* https://link.springer.com/article/10.1007/BF02377938
* [...]
https://en.wikipedia.org/wiki/Evania_appendigaster
"""
Evania appendigaster is a species of wasp in the family Evaniidae, the ensign wasps. Its native range is not known, but it likely originated in Asia. Today it occurs throughout the tropics and subtropics and in many temperate regions. It is a parasitoid wasp known for specializing on cockroaches.[1]
[...]
The wasp may be a candidate for use as an agent of biological pest control of cockroaches.[5][8] Control might be even better if the wasp were released along with A. hagenowii, which tends to have a higher rate of parasitism.[1]
"""
________________
another one!
https://en.wikipedia.org/wiki/Emerald_cockroach_wasp
"Ampulex compressa"
great:
* https://www.youtube.com/watch?v=ovo_T0KqdYg
* https://www.youtube.com/watch?v=-ySwuQhruBo
* [...]
________________
More on both species as "NATURAL ENEMIES":
* https://faculty.ucr.edu/~legneref/biotact/ch-27.htm
* https://link.springer.com/article/10.1007/BF02377938
* [...]
¶ECDC "VectorNet" monitoring tool
"""
ECDC and EFSA, through the VectorNet network, continues to improve the data collection for the maps. VectorNet is looking for vector-borne disease experts who are interested in sharing data on the distribution of mosquito, tick, sand fly and culicoides vectors. Experts can contact VectorNet at VectorNet@ecdc.europa.eu to join the network. They can also register and upload data to the common database through the VectorNet tool.
"""
via https://www.ecdc.europa.eu/en/publications-data/aedes-aegypti-current-known-distribution-europe-april-2017
__________
https://vectornet.ecdc.europa.eu/
"""
VectorNet is a joint initiative of the European Food Safety Authority (EFSA) and the European Centre for Disease Prevention and Control (ECDC), which started in May 2014. The Project supports the collection of data on vectors and pathogens in vectors, related to both animal and human health.
This tool allows you to submit information on the distribution of ticks, mosquitoes, sand flies and biting midges.
"""
"""
ECDC and EFSA, through the VectorNet network, continues to improve the data collection for the maps. VectorNet is looking for vector-borne disease experts who are interested in sharing data on the distribution of mosquito, tick, sand fly and culicoides vectors. Experts can contact VectorNet at VectorNet@ecdc.europa.eu to join the network. They can also register and upload data to the common database through the VectorNet tool.
"""
via https://www.ecdc.europa.eu/en/publications-data/aedes-aegypti-current-known-distribution-europe-april-2017
__________
https://vectornet.ecdc.europa.eu/
"""
VectorNet is a joint initiative of the European Food Safety Authority (EFSA) and the European Centre for Disease Prevention and Control (ECDC), which started in May 2014. The Project supports the collection of data on vectors and pathogens in vectors, related to both animal and human health.
This tool allows you to submit information on the distribution of ticks, mosquitoes, sand flies and biting midges.
"""
¶sandboxes (and sand beaches) are disguisting because cats shit in them
#anticats
https://www.wormsandgermsblog.com/files/2008/04/M3-Sandbox2.pdf
zoonotic diseases...
* "Cutaneous larval migrans" (hookworms)
* "Visceral and ocular larval migrans" (roundworms) ... "toxocara"
* toxoplasmosis via oocysts
#anticats
https://www.wormsandgermsblog.com/files/2008/04/M3-Sandbox2.pdf
zoonotic diseases...
* "Cutaneous larval migrans" (hookworms)
* "Visceral and ocular larval migrans" (roundworms) ... "toxocara"
* toxoplasmosis via oocysts
¶covid pandemic : mink->human vector
https://www.wormsandgermsblog.com/2020/05/articles/animals/other-animals/suspected-mink-to-human-transmission-of-sars-cov-2/
https://www.wormsandgermsblog.com/2020/05/articles/animals/other-animals/suspected-mink-to-human-transmission-of-sars-cov-2/
¶Report: CHT7A situation
Situation:
* We had stuff stored at a friend's place (#vaults)
* Another friends staying there reported weird bites - not just fleas (there were many dogs and cats living there)
* He suspected bed bugs (but never found any proof, and wouldn't know how)
We:
* After handling our stuff, we also had a period of weird bites
* kept a high lookout, but never found any source
* sprayed lots of tea tree oil
* After some time, it seemed to all be fine
* There seemed to be some recurrances when handling some packed-away items (sleeping bags), even though they have been washed in between
Explanation:
* might have been just one loose flea at our place, or some stuck spiders
* our friend probably just had fleas, or perhaps mites
* there was poultry at the place, and goats:
mites are possible!
* anyway, everything resolved itself
Situation:
* We had stuff stored at a friend's place (#vaults)
* Another friends staying there reported weird bites - not just fleas (there were many dogs and cats living there)
* He suspected bed bugs (but never found any proof, and wouldn't know how)
We:
* After handling our stuff, we also had a period of weird bites
* kept a high lookout, but never found any source
* sprayed lots of tea tree oil
* After some time, it seemed to all be fine
* There seemed to be some recurrances when handling some packed-away items (sleeping bags), even though they have been washed in between
Explanation:
* might have been just one loose flea at our place, or some stuck spiders
* our friend probably just had fleas, or perhaps mites
* there was poultry at the place, and goats:
mites are possible!
* anyway, everything resolved itself
¶Moths ?
* agricultural pest
* household pest
________________________
https://en.wikipedia.org/wiki/Depressariinae
http://europepmc.org/article/PMC/5523186
"Three new species and one new subspecies of Depressariinae (Lepidoptera) from Europe."
(found in Canarias)
_____________
* agricultural pest
* household pest
________________________
https://en.wikipedia.org/wiki/Depressariinae
http://europepmc.org/article/PMC/5523186
"Three new species and one new subspecies of Depressariinae (Lepidoptera) from Europe."
(found in Canarias)
_____________
¶Zoonosis
→ https://en.wikipedia.org/wiki/Zoonosis
"""
A zoonosis (plural zoonoses, or zoonotic diseases) is an infectious disease caused by a pathogen (an infectious agent, such as a bacterium, virus, parasite or prion) that has jumped from a non-human animal (usually a vertebrate) to a human.[1][2][3] Typically, the first infected human transmits the infectious agent to at least one other human, who, in turn, infects others.
"""
→ https://en.wikipedia.org/wiki/Zoonosis
"""
A zoonosis (plural zoonoses, or zoonotic diseases) is an infectious disease caused by a pathogen (an infectious agent, such as a bacterium, virus, parasite or prion) that has jumped from a non-human animal (usually a vertebrate) to a human.[1][2][3] Typically, the first infected human transmits the infectious agent to at least one other human, who, in turn, infects others.
"""
¶TICKS— Arbovirus (general term for arthropod-zoonotic diseases)
https://en.wikipedia.org/wiki/Arbovirus
"""
Arbovirus is an informal name used to refer to any viruses that are transmitted by arthropod vectors. The word arbovirus is an acronym (arthropod-borne virus).[1] The word tibovirus (tick-borne virus) is sometimes used to more specifically describe viruses transmitted by ticks, a superorder within the arthropods
"""
"""
Arboviruses maintain themselves in nature by going through a cycle between a host, an organism that carries the virus, and a vector, an organism that carries and transmits the virus to other organisms.[8] For arboviruses, vectors are commonly mosquitoes, ticks, sandflies[9] and other arthropods that consume the blood of vertebrates for nutritious or developmental purposes
"""
https://en.wikipedia.org/wiki/Arbovirus
"""
Arbovirus is an informal name used to refer to any viruses that are transmitted by arthropod vectors. The word arbovirus is an acronym (arthropod-borne virus).[1] The word tibovirus (tick-borne virus) is sometimes used to more specifically describe viruses transmitted by ticks, a superorder within the arthropods
"""
"""
Arboviruses maintain themselves in nature by going through a cycle between a host, an organism that carries the virus, and a vector, an organism that carries and transmits the virus to other organisms.[8] For arboviruses, vectors are commonly mosquitoes, ticks, sandflies[9] and other arthropods that consume the blood of vertebrates for nutritious or developmental purposes
"""
¶Bad for other species (plants, fish, livestock, ...)
ties to:
#Gardening / agriculture / farming pests! ← +KuM !!!
____________________
https://entomology.ca.uky.edu/content/entomology-master-gardeners-introduction :
>< gardening
https://en.wikipedia.org/wiki/Sea_louse :
>< fish
https://en.wikipedia.org/wiki/Phylloxera
"""
In the late 19th century the phylloxera epidemic destroyed most of the vineyards for wine grapes in Europe, most notably in France.[4] Phylloxera was introduced to Europe when avid botanists in Victorian England collected specimens of American vines in the 1850s
"""
<--------------- (new) pests for other species ↑
ties to:
#Gardening / agriculture / farming pests! ← +KuM !!!
____________________
https://entomology.ca.uky.edu/content/entomology-master-gardeners-introduction :
>< gardening
https://en.wikipedia.org/wiki/Sea_louse :
>< fish
https://en.wikipedia.org/wiki/Phylloxera
"""
In the late 19th century the phylloxera epidemic destroyed most of the vineyards for wine grapes in Europe, most notably in France.[4] Phylloxera was introduced to Europe when avid botanists in Victorian England collected specimens of American vines in the 1850s
"""
<--------------- (new) pests for other species ↑
¶Insects fossils
are pests the same as they used to be?
what's the evolution scheme of those?
can we trace it back in fossils?
how do you study past pests in places with no pines (so no amber) like Canarias?
https://www.alamy.com/stock-photo/fossilized-insect.html
are pests the same as they used to be?
what's the evolution scheme of those?
can we trace it back in fossils?
how do you study past pests in places with no pines (so no amber) like Canarias?
https://www.alamy.com/stock-photo/fossilized-insect.html
¶flies can spread mites
* i have this on microscope
* internet agrees
???:
* which ones could be dangerous
* is this like hitch-hiking? how does it happen?
* [...]
* i have this on microscope
* internet agrees
???:
* which ones could be dangerous
* is this like hitch-hiking? how does it happen?
* [...]
¶(check if all) more pets→pests zoonosis
:
* https://www.aler.si/clanki/bolezni-ki-jih-lahko-dobimo-od-svojega-psa-in-kako-se-pred-njimi-obvarovati.html
* [...]
:
* https://www.aler.si/clanki/bolezni-ki-jih-lahko-dobimo-od-svojega-psa-in-kako-se-pred-njimi-obvarovati.html
* [...]
¶on ivermectin
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3043740/
Ivermectin, ‘Wonder drug’ from Japan: the human use perspective
pretty amazing story!
"""
Discovered in the late-1970s, the pioneering drug ivermectin, a dihydro derivative of avermectin—originating solely from a single microorganism isolated at the Kitasato Intitute, Tokyo, Japan from Japanese soil—has had an immeasurably beneficial impact in improving the lives and welfare of billions of people throughout the world. Originally introduced as a veterinary drug, it kills a wide range of internal and external parasites in commercial livestock and companion animals. It was quickly discovered to be ideal in combating two of the world’s most devastating and disfiguring diseases which have plagued the world’s poor throughout the tropics for centuries. It is now being used free-of-charge as the sole tool in campaigns to eliminate both diseases globally. It has also been used to successfully overcome several other human diseases and new uses for it are continually being found. This paper looks in depth at the events surrounding ivermectin’s passage from being a huge success in Animal Health into its widespread use in humans, a development which has led many to describe it as a “wonder” drug.
Keywords: avermectin, ivermectin, mode of action, onchocerciasis, lymphatic filariasis, drug resistance
"""
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3043740/
Ivermectin, ‘Wonder drug’ from Japan: the human use perspective
pretty amazing story!
"""
Discovered in the late-1970s, the pioneering drug ivermectin, a dihydro derivative of avermectin—originating solely from a single microorganism isolated at the Kitasato Intitute, Tokyo, Japan from Japanese soil—has had an immeasurably beneficial impact in improving the lives and welfare of billions of people throughout the world. Originally introduced as a veterinary drug, it kills a wide range of internal and external parasites in commercial livestock and companion animals. It was quickly discovered to be ideal in combating two of the world’s most devastating and disfiguring diseases which have plagued the world’s poor throughout the tropics for centuries. It is now being used free-of-charge as the sole tool in campaigns to eliminate both diseases globally. It has also been used to successfully overcome several other human diseases and new uses for it are continually being found. This paper looks in depth at the events surrounding ivermectin’s passage from being a huge success in Animal Health into its widespread use in humans, a development which has led many to describe it as a “wonder” drug.
Keywords: avermectin, ivermectin, mode of action, onchocerciasis, lymphatic filariasis, drug resistance
"""
¶Fibiger 1926 Nobel prize for medicine fail : "Roundworms causing cancer"
https://en.wikipedia.org/wiki/Johannes_Fibiger
"""
After his death, independent researches proved that G. neoplasticum cannot cause cancer. Tumours and cancer produced by Fibiger were due to vitamin A deficiency. Historical reassessment of Fibiger's data revealed that he had mistaken non-cancerous tumours for cancerous tumours.
"""
https://ebrary.net/93514/health/hunting_cancer_microbe
https://en.wikipedia.org/wiki/Johannes_Fibiger
"""
After his death, independent researches proved that G. neoplasticum cannot cause cancer. Tumours and cancer produced by Fibiger were due to vitamin A deficiency. Historical reassessment of Fibiger's data revealed that he had mistaken non-cancerous tumours for cancerous tumours.
"""
https://ebrary.net/93514/health/hunting_cancer_microbe
¶BIOWEAPONS/USSR— Biological warfare
"""
Over the course of its history, the Soviet program is known to have weaponized and stockpiled the following eleven bio-agents[3] (and to have pursued basic research on many more):
"""
Over the course of its history, the Soviet program is known to have weaponized and stockpiled the following eleven bio-agents[3] (and to have pursued basic research on many more):
- Bacillus anthracis (anthrax)[4]
- Yersinia pestis (plague)[4]
- Francisella tularensis (tularemia)
- Burkholderia mallei (glanders)
- Brucella sp. (brucellosis)
- Coxiella burnetii (Q-fever)
- Venezuelan equine encephalitis virus (VEE)
- Botulinum toxin
- Staphylococcal enterotoxin B
- Smallpox[4]
- Marburg virus
- Orthopoxvirus[4]These programs became immense and were conducted at dozens of secret sites employing up to 65,000 people.[1] Annualized production capacity for weaponized smallpox, for example, was 90 to 100 tons.
¶BIOWEAPONS— "Chimera Project"
"""
The Chimera Project attempted in the late 1980s and early 1990s to combine DNA from Venezuelan equine encephalitis and smallpox at Obolensk, and Ebola virus and smallpox at Vector. The existence of these chimeric viruses programmes was one reason why Alibek defected to the United States in 1992. Journal articles by scientists suggest that in 1999 the experiments were still being continued.[27][43]
"""
"""
The Chimera Project attempted in the late 1980s and early 1990s to combine DNA from Venezuelan equine encephalitis and smallpox at Obolensk, and Ebola virus and smallpox at Vector. The existence of these chimeric viruses programmes was one reason why Alibek defected to the United States in 1992. Journal articles by scientists suggest that in 1999 the experiments were still being continued.[27][43]
"""
¶WARFARE/BIOWEAPONS— "Entomological warfare"
https://en.wikipedia.org/wiki/Entomological_warfare
https://en.wikipedia.org/wiki/United_States_biological_weapons_program#Korean_War
https://en.wikipedia.org/wiki/Operation_Drop_Kick
https://en.wikipedia.org/wiki/Operation_May_Day
https://en.wikipedia.org/wiki/Operation_Big_Itch
https://en.wikipedia.org/wiki/Entomological_warfare
https://en.wikipedia.org/wiki/United_States_biological_weapons_program#Korean_War
https://en.wikipedia.org/wiki/Operation_Drop_Kick
https://en.wikipedia.org/wiki/Operation_May_Day
https://en.wikipedia.org/wiki/Operation_Big_Itch
¶BIOWEAPONS— Brucellosis
https://www.cdc.gov/brucellosis/index.html
(mentioned by Lavrov as being investigated in US/Ukraine biolabs, 2022/03)
https://www.cdc.gov/brucellosis/index.html
(mentioned by Lavrov as being investigated in US/Ukraine biolabs, 2022/03)
¶Pine processionary
https://en.wikipedia.org/wiki/Pine_processionary
"hrastov prelec"
Thaumetopoca pityocompa
https://www.24ur.com/specialno/nega_in_zdravje/majhne-kosmate-in-ne-tako-nedolzne.html
https://www.bakos.si/uncategorized/smrtno-nevarna-kosmata-gosenica-lahko-zadusi-psa/
https://en.wikipedia.org/wiki/Pine_processionary
"hrastov prelec"
Thaumetopoca pityocompa
https://www.24ur.com/specialno/nega_in_zdravje/majhne-kosmate-in-ne-tako-nedolzne.html
https://www.bakos.si/uncategorized/smrtno-nevarna-kosmata-gosenica-lahko-zadusi-psa/
¶Antibiotics
see → 🔗medical
https://en.wikipedia.org/wiki/Metronidazole (Flagyl/Efloran)
"""
Metronidazole, marketed under the brand name Flagyl among others, is an antibiotic and antiprotozoal medication.[4] It is used either alone or with other antibiotics to treat pelvic inflammatory disease, endocarditis, and bacterial vaginosis.[4] It is effective for dracunculiasis, giardiasis, trichomoniasis, and amebiasis.[4] It is an option for a first episode of mild-to-moderate Clostridium difficile colitis if vancomycin or fidaxomicin is unavailable.[4][5] Metronidazole is available by mouth, as a cream, and by injection into a vein.[4]
"""
https://www.krka.si/sl/zdravila-in-izdelki/zdravila-na-recept/efloran/1321/
see → 🔗medical
https://en.wikipedia.org/wiki/Metronidazole (Flagyl/Efloran)
"""
Metronidazole, marketed under the brand name Flagyl among others, is an antibiotic and antiprotozoal medication.[4] It is used either alone or with other antibiotics to treat pelvic inflammatory disease, endocarditis, and bacterial vaginosis.[4] It is effective for dracunculiasis, giardiasis, trichomoniasis, and amebiasis.[4] It is an option for a first episode of mild-to-moderate Clostridium difficile colitis if vancomycin or fidaxomicin is unavailable.[4][5] Metronidazole is available by mouth, as a cream, and by injection into a vein.[4]
"""
https://www.krka.si/sl/zdravila-in-izdelki/zdravila-na-recept/efloran/1321/
¶Cronobacter sakazakii (in USA baby formula)
https://www.wsws.org/en/articles/2022/05/28/mzvs-m28.html
"""
Califf also reported leaks in the roof, standing water in the factory and two instances in the past, based on internal company documents, when finished baby formula was known to have “environmental contamination with Cronobacter sakazakii.” The FDA commissioner claimed that these poisoned batches, which were produced by Abbott Labs in 2019 and 2020, had been destroyed by the company.
"""
https://www.wsws.org/en/articles/2022/05/28/mzvs-m28.html
"""
Califf also reported leaks in the roof, standing water in the factory and two instances in the past, based on internal company documents, when finished baby formula was known to have “environmental contamination with Cronobacter sakazakii.” The FDA commissioner claimed that these poisoned batches, which were produced by Abbott Labs in 2019 and 2020, had been destroyed by the company.
"""
¶"Valley fever" (fungal, by Coccidioidomycosis)
https://www.theguardian.com/us-news/2022/aug/29/california-valley-fever-disease-climate-crisis
###
https://www.cdc.gov/fungal/diseases/coccidioidomycosis/index.html
https://www.cdc.gov/fungal/diseases/coccidioidomycosis/definition.html
"""
Valley fever is an infection caused by the fungus Coccidioides. The scientific name for Valley fever is “coccidioidomycosis,” and it’s also sometimes called “San Joaquin Valley fever” or “desert rheumatism.” The term “Valley fever” usually refers to Coccidioides infection in the lungs, but the infection can spread to other parts of the body in severe cases (this is called “disseminated coccidioidomycosis”).
"""
https://www.theguardian.com/us-news/2022/aug/29/california-valley-fever-disease-climate-crisis
###
https://www.cdc.gov/fungal/diseases/coccidioidomycosis/index.html
https://www.cdc.gov/fungal/diseases/coccidioidomycosis/definition.html
"""
Valley fever is an infection caused by the fungus Coccidioides. The scientific name for Valley fever is “coccidioidomycosis,” and it’s also sometimes called “San Joaquin Valley fever” or “desert rheumatism.” The term “Valley fever” usually refers to Coccidioides infection in the lungs, but the infection can spread to other parts of the body in severe cases (this is called “disseminated coccidioidomycosis”).
"""
¶[s!!] great veterinary list
https://www.uradni-list.si/glasilo-uradni-list-rs/vsebina/11105
"""
5. člen
V tretjo skupino spadajo bolezni, ki so zelo nalezljive. Širjenje teh bolezni se med rejami lahko prepreči z ustreznimi veterinarsko-sanitarnimi ukrepi. Te bolezni povzročajo velike ekonomske škode in ogrožajo obstoj posamezne živalske vrste. Metode preprečevanja pojavov in širjenja ter izkoreninjenja teh bolezni so poznane in se jih da izvajati.
Diagnostične preiskave, preventivne vakcinacije in izkoreninjenje z odškodninami za pobite živali ob izpolnitvi predpisanih pogojev se plačujejo iz proračuna Republike Slovenije. V primeru okuženosti reje se živali neškodljivo uničijo in se prepove promet z živalmi, izdelki in surovinami živalskega izvora.
Bolezni tretje skupine so:
– afriška prašičja kuga – Pestis africana suum,
– atipična kokošja kuga – Morbus Newcastle (Newcastle disease),
– bolezen Aujeszkega – Morbus Aujeszky,
– bolezen modrikastega jezika – Febris catarrhalis ovium (Blue tongue),
– bruceloza – Brucellosis (B. melitensis, abortus in suis),
– goveja kuga – Pestis bovina (Rinderpest),
– goveja spongiformna encefalopatija – Encephalophatia spongiformis bovum,
– hemoragična septikemija pri govedu – Septicemia haemorrhagica bovum,
– klasična prašičja kuga – Pestis suum,
– kokošja kuga – Pestis avium,
– konjska kuga – Pestis equorum,
– kuga drobnice – Pestis pecorum,
– mrzlica doline Rift – Hepatitis infectiosa enzootica bovum et ovium,
– nalezljiva kuga goved – Pleuropneumonia contagiosa bovum,
– slinavka in parkljevka – Aphtae epizooticae,
– spolna kuga konj – Exanthema coitale paralyticum (Durina),
– vezikularna bolezen prašičev – Morbus vesicularis suum,
– vezikularni stomatitis – Stomatitis vesicularis in
– vozličasti dermatitis – Dermatitis nodosa.
6. člen
V skupino zoonoz spadajo bolezni, ki so nevarne ljudem in živalim in se po naravni poti prenašajo z živali – vretenčarjev na ljudi in obratno. Glede na lastnosti ter pogoje so lahko razvrščene v prvo, drugo in tretjo skupino bolezni.
– bruceloza – Brucellosis (razen B. Ovis),
– cisticerkoza – Cysticercosis,
– ehinokokoza – Echinococosis,
– leptospiroza – Leptospirosis,
– listerioza – Listeriosis,
– mikrosporija – Microsporiasis,
– mrzlica doline Rift – Hepatitis infectiosa enzootica bovum et ovium,
– mrzlica Q – Q febris, .......... ("Q fever", via ticks!, also in Cuba)
– okamenela zalega – Aspergillosis apium,
– psitakoza – Psittacosis,
– rdečica – Erysipelas,
– salmoneloza – Salmonellosis,
– smrkavost – Malleus,
– steklina – Rabies (Lyssa),
– toksoplazmoza – Toxoplasmosis,
– trihineloza –. Trichinellosis,
– trihofitija – Trichophytia bovis,
– tuberkuloza – Tuberculosis in
– tularemija – Tularemia.
7. člen
Kužne bolezni, ki jih je treba ugotoviti takoj oziroma je treba takoj ugotoviti vzrok pogina, so:
– vse bolezni iz tretje skupine in
– vse zoonoze.
"""
https://www.uradni-list.si/glasilo-uradni-list-rs/vsebina/11105
"""
5. člen
V tretjo skupino spadajo bolezni, ki so zelo nalezljive. Širjenje teh bolezni se med rejami lahko prepreči z ustreznimi veterinarsko-sanitarnimi ukrepi. Te bolezni povzročajo velike ekonomske škode in ogrožajo obstoj posamezne živalske vrste. Metode preprečevanja pojavov in širjenja ter izkoreninjenja teh bolezni so poznane in se jih da izvajati.
Diagnostične preiskave, preventivne vakcinacije in izkoreninjenje z odškodninami za pobite živali ob izpolnitvi predpisanih pogojev se plačujejo iz proračuna Republike Slovenije. V primeru okuženosti reje se živali neškodljivo uničijo in se prepove promet z živalmi, izdelki in surovinami živalskega izvora.
Bolezni tretje skupine so:
– afriška prašičja kuga – Pestis africana suum,
– atipična kokošja kuga – Morbus Newcastle (Newcastle disease),
– bolezen Aujeszkega – Morbus Aujeszky,
– bolezen modrikastega jezika – Febris catarrhalis ovium (Blue tongue),
– bruceloza – Brucellosis (B. melitensis, abortus in suis),
– goveja kuga – Pestis bovina (Rinderpest),
– goveja spongiformna encefalopatija – Encephalophatia spongiformis bovum,
– hemoragična septikemija pri govedu – Septicemia haemorrhagica bovum,
– klasična prašičja kuga – Pestis suum,
– kokošja kuga – Pestis avium,
– konjska kuga – Pestis equorum,
– kuga drobnice – Pestis pecorum,
– mrzlica doline Rift – Hepatitis infectiosa enzootica bovum et ovium,
– nalezljiva kuga goved – Pleuropneumonia contagiosa bovum,
– slinavka in parkljevka – Aphtae epizooticae,
– spolna kuga konj – Exanthema coitale paralyticum (Durina),
– vezikularna bolezen prašičev – Morbus vesicularis suum,
– vezikularni stomatitis – Stomatitis vesicularis in
– vozličasti dermatitis – Dermatitis nodosa.
6. člen
V skupino zoonoz spadajo bolezni, ki so nevarne ljudem in živalim in se po naravni poti prenašajo z živali – vretenčarjev na ljudi in obratno. Glede na lastnosti ter pogoje so lahko razvrščene v prvo, drugo in tretjo skupino bolezni.
– bruceloza – Brucellosis (razen B. Ovis),
– cisticerkoza – Cysticercosis,
– ehinokokoza – Echinococosis,
– leptospiroza – Leptospirosis,
– listerioza – Listeriosis,
– mikrosporija – Microsporiasis,
– mrzlica doline Rift – Hepatitis infectiosa enzootica bovum et ovium,
– mrzlica Q – Q febris, .......... ("Q fever", via ticks!, also in Cuba)
– okamenela zalega – Aspergillosis apium,
– psitakoza – Psittacosis,
– rdečica – Erysipelas,
– salmoneloza – Salmonellosis,
– smrkavost – Malleus,
– steklina – Rabies (Lyssa),
– toksoplazmoza – Toxoplasmosis,
– trihineloza –. Trichinellosis,
– trihofitija – Trichophytia bovis,
– tuberkuloza – Tuberculosis in
– tularemija – Tularemia.
7. člen
Kužne bolezni, ki jih je treba ugotoviti takoj oziroma je treba takoj ugotoviti vzrok pogina, so:
– vse bolezni iz tretje skupine in
– vse zoonoze.
"""
¶[!!*] Dengue in Europe
https://www.euronews.com/green/2024/06/13/which-european-countries-have-tiger-mosquitoes-dengue-cases-are-rising-with-temperatures
"""
There were 130 locally acquired cases of dengue fever in the EU last year, compared to 71 cases in 2022, the European Centre for Disease Prevention and Control (ECDC) revealed this week.
There has been a recent spike in cases in Europe, with the invasive mosquito species found in 13 EU countries.
"""
"""
The yellow fever mosquito - also a vector of dengue, chikungunya, and Zika viruses - made its way to Cyprus in 2022.
"""
https://www.euronews.com/green/2024/06/13/which-european-countries-have-tiger-mosquitoes-dengue-cases-are-rising-with-temperatures
"""
There were 130 locally acquired cases of dengue fever in the EU last year, compared to 71 cases in 2022, the European Centre for Disease Prevention and Control (ECDC) revealed this week.
There has been a recent spike in cases in Europe, with the invasive mosquito species found in 13 EU countries.
"""
"""
The yellow fever mosquito - also a vector of dengue, chikungunya, and Zika viruses - made its way to Cyprus in 2022.
"""
¶Helicobacter pylori → stomach cancers
https://en.wikipedia.org/wiki/Helicobacter_pylori
"""
Helicobacter pylori, previously known as Campylobacter pylori, is a gram-negative, flagellated, helical bacterium. Mutants can have a rod or curved rod shape, and these are less effective.[1][2] Its helical body (from which the genus name, Helicobacter, derives) is thought to have evolved in order to penetrate the mucous lining of the stomach, helped by its flagella, and thereby establish infection.[3][2] The bacterium was first identified as the causal agent of gastric ulcers in 1983 by the Australian doctors Barry Marshall and Robin Warren.[4][5]
"""
causing cancer
"""
Helicobacter pylori is a class 1 carcinogen, and potential cancers include gastric mucosa-associated lymphoid tissue (MALT) lymphomas and gastric cancer.[9][10] Infection with H. pylori is responsible for around 89 per cent of all gastric cancers, and is linked to the development of 5.5 per cent of all cases of cancer worldwide.[12][13] H. pylori is the only bacterium known to cause cancer.[14]
"""
------------
#diagnostics
Slovenia 2024 program of screening for mid 30s people.
https://en.wikipedia.org/wiki/Helicobacter_pylori
"""
Helicobacter pylori, previously known as Campylobacter pylori, is a gram-negative, flagellated, helical bacterium. Mutants can have a rod or curved rod shape, and these are less effective.[1][2] Its helical body (from which the genus name, Helicobacter, derives) is thought to have evolved in order to penetrate the mucous lining of the stomach, helped by its flagella, and thereby establish infection.[3][2] The bacterium was first identified as the causal agent of gastric ulcers in 1983 by the Australian doctors Barry Marshall and Robin Warren.[4][5]
"""
causing cancer
"""
Helicobacter pylori is a class 1 carcinogen, and potential cancers include gastric mucosa-associated lymphoid tissue (MALT) lymphomas and gastric cancer.[9][10] Infection with H. pylori is responsible for around 89 per cent of all gastric cancers, and is linked to the development of 5.5 per cent of all cases of cancer worldwide.[12][13] H. pylori is the only bacterium known to cause cancer.[14]
"""
------------
#diagnostics
Slovenia 2024 program of screening for mid 30s people.
¶[!!] Fox poo → Fox tapeworm (Echinococcus multilocularis)
https://en.wikipedia.org/wiki/Echinococcus_multilocularis
"""
The disease has extended its range in Europe in the last few decades.[15] Still the infection is fairly rare. Between 1982 and 2000 a total of 559 cases were reported throughout Europe.[16]
[...]
If no specific therapy is initiated, in 94% of patients the disease is fatal within 10–20 years following diagnosis.[10]
"""
* 3-6 mm long (when grown up)
"""
B67.7
Okužba, ki jo povzroča Echinococcus multilocularis, neopredeljena
Echinococcosis multilocularis, non specificata
"""
-------------------------
"""
Foxes, coyotes, domestic dogs, and other canids are the definitive hosts for the adult stage of the parasite.
Cats may also be involved
"""
wow okay #toxoplasmosis #anticats
-------------------------------
"""
due to limited knowledge about the parasite, it is often not monitored in wild or domestic animals; this monitoring will become crucial to the control of the parasite in the future as it continues to spread
"""
https://en.wikipedia.org/wiki/Echinococcus_multilocularis
"""
The disease has extended its range in Europe in the last few decades.[15] Still the infection is fairly rare. Between 1982 and 2000 a total of 559 cases were reported throughout Europe.[16]
[...]
If no specific therapy is initiated, in 94% of patients the disease is fatal within 10–20 years following diagnosis.[10]
"""
* 3-6 mm long (when grown up)
"""
B67.7
Okužba, ki jo povzroča Echinococcus multilocularis, neopredeljena
Echinococcosis multilocularis, non specificata
"""
-------------------------
"""
Foxes, coyotes, domestic dogs, and other canids are the definitive hosts for the adult stage of the parasite.
Cats may also be involved
"""
wow okay #toxoplasmosis #anticats
-------------------------------
"""
due to limited knowledge about the parasite, it is often not monitored in wild or domestic animals; this monitoring will become crucial to the control of the parasite in the future as it continues to spread
"""
¶Anopheles gambiae mosquito → Wuchereria bancrofti → Lymphatic philariasis (elephantiasis tropica)
ties to lynch's "elephant man" (not really)
ties to #cuba
https://en.wikipedia.org/wiki/Lymphatic_filariasis
"""
Lymphatic filariasis is a human disease caused by parasitic worms known as filarial worms.[2][3] Usually acquired in childhood, it is a leading cause of permanent disability worldwide, impacting over a hundred million people and manifesting itself in a variety of severe clinical pathologies[6][7] While most cases have no symptoms, some people develop a syndrome called elephantiasis, which is marked by severe swelling in the arms, legs, breasts, or genitals. The skin may become thicker as well, and the condition may become painful.[2] Affected people are often unable to work and are often shunned or rejected by others because of their disfigurement and disability.[7]
It is the first of the mosquito-borne diseases to have been identified.[8] The worms are spread by the bites of infected mosquitoes.[2] Three types of worms are known to cause the disease: Wuchereria bancrofti, Brugia malayi, and Brugia timori, with Wuchereria bancrofti being the most common.[2]
"""
https://en.wikipedia.org/wiki/Lymphatic_filariasis
"""
Lymphatic filariasis is a human disease caused by parasitic worms known as filarial worms.[2][3] Usually acquired in childhood, it is a leading cause of permanent disability worldwide, impacting over a hundred million people and manifesting itself in a variety of severe clinical pathologies[6][7] While most cases have no symptoms, some people develop a syndrome called elephantiasis, which is marked by severe swelling in the arms, legs, breasts, or genitals. The skin may become thicker as well, and the condition may become painful.[2] Affected people are often unable to work and are often shunned or rejected by others because of their disfigurement and disability.[7]
It is the first of the mosquito-borne diseases to have been identified.[8] The worms are spread by the bites of infected mosquitoes.[2] Three types of worms are known to cause the disease: Wuchereria bancrofti, Brugia malayi, and Brugia timori, with Wuchereria bancrofti being the most common.[2]
"""
¶WORMS— ("helmintic infections" == parasitic worms)
aka "helminths"
https://en.wikipedia.org/wiki/Parasitic_worm
"""
Parasitic worms, also known as helminths,[1] are large macroparasites; adults can generally be seen with the naked eye. Many are intestinal worms that are soil-transmitted and infect the gastrointestinal tract. Other parasitic worms such as schistosomes reside in blood vessels.
Some parasitic worms, including leeches and monogeneans, are ectoparasites – thus, they are not classified as helminths, which are endoparasites.
"""
----------------
"""
Helminths are a group of organisms which share a similar form but are not necessarily evolutionarily related. The term "helminth" is an artificial term.[5][6] There is no real consensus on the taxonomy (or groupings) of the helminths, particularly within the nematodes.[7] The term "helminth" contains a number of phyla, many of which are completely unrelated. However, for practical considerations the term is currently used to describe four phyla with superficial similarities: Annelida (ringed or segmented worms), Platyhelminthes (flatworms), Nematoda (roundworms), and Acanthocephala (thorny-headed worms).[7] The phylum Platyhelminthes includes two classes of worms of particular medical significance: the cestodes (tapeworms) and the trematodes (flukes and blood flukes), depending on whether or not they have segmented bodies.[1][8]
"""
https://en.wikipedia.org/wiki/Helminthiasis
"""
Helminthiasis, also known as worm infection, is any macroparasitic disease of humans and other animals in which a part of the body is infected with parasitic worms, known as helminths. There are numerous species of these parasites, which are broadly classified into tapeworms, flukes, and roundworms. They often live in the gastrointestinal tract of their hosts, but they may also burrow into other organs, where they induce physiological damage.
[...]
Of all the known helminth species, the most important helminths with respect to understanding their transmission pathways, their control, inactivation and enumeration in samples of human excreta from dried feces, faecal sludge, wastewater, and sewage sludge are:[7]
Roundworm infection (nematodiasis)
________________________ [s!→]
THERAPY *WITH* WORMS ... (COEVOLUTION!)
https://www.helminthictherapywiki.org/wiki/Helminthic_Therapy_Wiki
"""
This is the world’s largest information database documenting the science, management, experience and results of helminth replacement, a form of probiotic self-treatment - not a medical treatment - that is also known as worm therapy, helminth therapy and helminthic therapy.
Solid scientific evidence shows that millions of years of co-evolution have created a symbiotic relationship between humans and helminths that provides us with essential immune regulation.
All immunocompetent humans need regular exposure to helminths in order to maintain optimal immune function and avoid risk for inflammation-associated disease… access to helminths is a basic human need. [1]
"""
###
aka "helminths"
https://en.wikipedia.org/wiki/Parasitic_worm
"""
Parasitic worms, also known as helminths,[1] are large macroparasites; adults can generally be seen with the naked eye. Many are intestinal worms that are soil-transmitted and infect the gastrointestinal tract. Other parasitic worms such as schistosomes reside in blood vessels.
Some parasitic worms, including leeches and monogeneans, are ectoparasites – thus, they are not classified as helminths, which are endoparasites.
"""
----------------
"""
Helminths are a group of organisms which share a similar form but are not necessarily evolutionarily related. The term "helminth" is an artificial term.[5][6] There is no real consensus on the taxonomy (or groupings) of the helminths, particularly within the nematodes.[7] The term "helminth" contains a number of phyla, many of which are completely unrelated. However, for practical considerations the term is currently used to describe four phyla with superficial similarities: Annelida (ringed or segmented worms), Platyhelminthes (flatworms), Nematoda (roundworms), and Acanthocephala (thorny-headed worms).[7] The phylum Platyhelminthes includes two classes of worms of particular medical significance: the cestodes (tapeworms) and the trematodes (flukes and blood flukes), depending on whether or not they have segmented bodies.[1][8]
"""
https://en.wikipedia.org/wiki/Helminthiasis
"""
Helminthiasis, also known as worm infection, is any macroparasitic disease of humans and other animals in which a part of the body is infected with parasitic worms, known as helminths. There are numerous species of these parasites, which are broadly classified into tapeworms, flukes, and roundworms. They often live in the gastrointestinal tract of their hosts, but they may also burrow into other organs, where they induce physiological damage.
[...]
Of all the known helminth species, the most important helminths with respect to understanding their transmission pathways, their control, inactivation and enumeration in samples of human excreta from dried feces, faecal sludge, wastewater, and sewage sludge are:[7]
- soil-transmitted helminths, including Ascaris lumbricoides (the most common worldwide), Trichuris trichiura, Necator americanus, Strongyloides stercoralis and Ancylostoma duodenale
- Hymenolepis nana
- Taenia saginata
- Enterobius
- Fasciola hepatica
- Schistosoma mansoni
- Toxocara canis
- Toxocara cati
Roundworm infection (nematodiasis)
- Filariasis (Wuchereria bancrofti, Brugia malayi infection)
- Onchocerciasis (Onchocerca volvulus infection)
- Soil-transmitted helminthiasis – this includes ascariasis (Ascaris lumbricoides infection), trichuriasis (Trichuris infection), and hookworm infection (includes necatoriasis and Ancylostoma duodenale infection)
- Trichostrongyliasis (Trichostrongylus spp. infection)
- Dracunculiasis (guinea worm infection)
- Baylisascaris (raccoon roundworm, may be transmitted to pets, livestock, and humans)
- Echinococcosis (Echinococcus infection)
- Hymenolepiasis (Hymenolepis infection)
- Taeniasis/cysticercosis (Taenia infection)
- Coenurosis (T. multiceps, T. serialis, T. glomerata, and T. brauni infection)
- Amphistomiasis (amphistomes infection)
- Clonorchiasis (Clonorchis sinensis infection)
- Fascioliasis (Fasciola infection)
- Fasciolopsiasis (Fasciolopsis buski infection)
- Opisthorchiasis (Opisthorchis infection)
- Paragonimiasis (Paragonimus infection)
- Schistosomiasis/bilharziasis (Schistosoma infection)
- Moniliformis infection
________________________ [s!→]
THERAPY *WITH* WORMS ... (COEVOLUTION!)
https://www.helminthictherapywiki.org/wiki/Helminthic_Therapy_Wiki
"""
This is the world’s largest information database documenting the science, management, experience and results of helminth replacement, a form of probiotic self-treatment - not a medical treatment - that is also known as worm therapy, helminth therapy and helminthic therapy.
Solid scientific evidence shows that millions of years of co-evolution have created a symbiotic relationship between humans and helminths that provides us with essential immune regulation.
All immunocompetent humans need regular exposure to helminths in order to maintain optimal immune function and avoid risk for inflammation-associated disease… access to helminths is a basic human need. [1]
"""
###
¶CUBA!— mosquito → (parasite→worm) → FILIARISIS / ELEPHANTITIS
TLDR:
* need "several bites in duration of several weeks/months" so "short term tourists are not endangered"
source ###
* could be eradicated with all taking medicine at same time
* can take years to show up
* "DEC" medicine can deactivate it, "taken yearly", in patients
* blood testing (for worm) is complicated, serum also unreliable
CUBA:
* Cuba is *NOT* shown in WHO's list of countries where it's present!?
* [!!] sharing house with patient: is this ... okay? without discussion/disclosure?:
↓↓
update: turned out a false alarm :D
* ###
TLDR:
* need "several bites in duration of several weeks/months" so "short term tourists are not endangered"
source ###
* could be eradicated with all taking medicine at same time
* can take years to show up
* "DEC" medicine can deactivate it, "taken yearly", in patients
* blood testing (for worm) is complicated, serum also unreliable
CUBA:
* Cuba is *NOT* shown in WHO's list of countries where it's present!?
* [!!] sharing house with patient: is this ... okay? without discussion/disclosure?:
↓↓
update: turned out a false alarm :D
* ###
¶[!!**t] Ultrasound pest disturbers (are probably a scam and dangerous)
Q @ruth.asomada:
* how does it impact the dogs and cats here?
* how does it impact the children (who hear higher pitch?)
* I definitely feel I got tinnitus from it
* how much exposure is needed to (by any account) suffer damage?
* ###
https://pmc.ncbi.nlm.nih.gov/articles/PMC4786042/
"""
For over 40 years, there have been reports of hearing threshold shift [1] and a range of subjective effects (nausea, dizziness, migraine, fatigue, tinnitus and ‘pressure in the ears’ [1]–[8]) from ultrasound in air to which workers have been routinely exposed (plus other symptoms that have not occurred in more than one study; §3b). The degree of response, from significant to none, varied between workers. The evidence base has not studied sufficient numbers of subjects, and has not been sufficiently sensitive to the presence of sensitive individuals, or sensitive subgroups, within the population, to support the guidelines required today
"""
Q @ruth.asomada:
* how does it impact the dogs and cats here?
* how does it impact the children (who hear higher pitch?)
* I definitely feel I got tinnitus from it
* how much exposure is needed to (by any account) suffer damage?
* ###
https://pmc.ncbi.nlm.nih.gov/articles/PMC4786042/
"""
For over 40 years, there have been reports of hearing threshold shift [1] and a range of subjective effects (nausea, dizziness, migraine, fatigue, tinnitus and ‘pressure in the ears’ [1]–[8]) from ultrasound in air to which workers have been routinely exposed (plus other symptoms that have not occurred in more than one study; §3b). The degree of response, from significant to none, varied between workers. The evidence base has not studied sufficient numbers of subjects, and has not been sufficiently sensitive to the presence of sensitive individuals, or sensitive subgroups, within the population, to support the guidelines required today
"""
¶Coxsackievirus
https://en.wikipedia.org/wiki/Coxsackievirus
* water-borne virus
"""
Coxsackieviruses are a few related enteroviruses that belong to the Picornaviridae family of nonenveloped, linear, positive-sense single-stranded RNA viruses, as well as its genus Enterovirus, which also includes poliovirus and echovirus. Enteroviruses are among the most common and important human pathogens, and ordinarily its members are transmitted by the fecal–oral route. Coxsackieviruses share many characteristics with poliovirus. With control of poliovirus infections in much of the world, more attention has been focused on understanding the nonpolio enteroviruses such as coxsackievirus. Coxsackieviruses are among the leading causes of aseptic meningitis (the other usual suspects being echovirus and mumps virus). [...] In 2007, an outbreak of coxsackievirus occurred in eastern China. It has been reported that 22 children died. More than 800 people were affected, with 200 children hospitalized.[18]"""
https://en.wikipedia.org/wiki/Coxsackievirus
* water-borne virus
"""
Coxsackieviruses are a few related enteroviruses that belong to the Picornaviridae family of nonenveloped, linear, positive-sense single-stranded RNA viruses, as well as its genus Enterovirus, which also includes poliovirus and echovirus. Enteroviruses are among the most common and important human pathogens, and ordinarily its members are transmitted by the fecal–oral route. Coxsackieviruses share many characteristics with poliovirus. With control of poliovirus infections in much of the world, more attention has been focused on understanding the nonpolio enteroviruses such as coxsackievirus. Coxsackieviruses are among the leading causes of aseptic meningitis (the other usual suspects being echovirus and mumps virus). [...] In 2007, an outbreak of coxsackievirus occurred in eastern China. It has been reported that 22 children died. More than 800 people were affected, with 200 children hospitalized.[18]"""
¶[!!] WATER/PROTECT— Water filters (and their limits, problems)
* does it even make sense to carry non-virus filtering filters???
* does it even make sense to carry non-virus filtering filters???
¶TICKS– Babesios
https://en.wikipedia.org/wiki/Babesiosis
"""
(PRESENTATION)
After trypanosomes, Babesia is thought to be the second-most common blood parasite of mammals
People with symptoms usually become ill 1 to 4 weeks after the bite,
[...]
(TREATMENT)
Treatment of asymptomatic carriers should be considered if parasites are still detected after 3 months. In mild-to-moderate babesiosis, the treatment of choice is a combination of atovaquone and azithromycin. This regimen is preferred to clindamycin and quinine because it has fewer side effects. The standard course is 7 to 10 days, but this is extended to at least 6 weeks in people with relapsing disease.
"""
"""
Babesia species are in the phylum Apicomplexa, which also has the protozoan parasites that cause malaria, toxoplasmosis, and cryptosporidiosis.[5] Four clades of Babesia species infect humans. The main species in each clade are:[citation needed]
Babesia parasites reproduce in red blood cells, where they can be seen as cross-shaped inclusions (four merozoites asexually budding, but attached forming a structure looking like a "Maltese cross")[11] and cause hemolytic anemia, quite similar to malaria.
------------
Only specialized laboratories can adequately diagnose Babesia infection in humans, so Babesia infections are considered highly under-reported. [...] It develops in patients who live in or travel to an endemic area or receive a contaminated blood transfusion within the preceding 9 weeks, so this aspect of the medical history is vital.[13] Babesiosis may be suspected when a person with such an exposure history develops persistent fevers and hemolytic anemia. The definitive diagnostic test is the identification of parasites on a Giemsa-stained thin-film blood smear.[13]
------------
"""
https://en.wikipedia.org/wiki/Babesiosis
"""
(PRESENTATION)
After trypanosomes, Babesia is thought to be the second-most common blood parasite of mammals
People with symptoms usually become ill 1 to 4 weeks after the bite,
[...]
(TREATMENT)
Treatment of asymptomatic carriers should be considered if parasites are still detected after 3 months. In mild-to-moderate babesiosis, the treatment of choice is a combination of atovaquone and azithromycin. This regimen is preferred to clindamycin and quinine because it has fewer side effects. The standard course is 7 to 10 days, but this is extended to at least 6 weeks in people with relapsing disease.
"""
"""
Babesia species are in the phylum Apicomplexa, which also has the protozoan parasites that cause malaria, toxoplasmosis, and cryptosporidiosis.[5] Four clades of Babesia species infect humans. The main species in each clade are:[citation needed]
- B. microti (< 3 μm)
- B. duncani
- B. divergens (cattle parasite seen mostly in Europe) and B. venatorum (roe deer parasite, formerly called EU1), most closely related to the large Babesia clade
- Large Babesia (> 3 μm) mostly infects ungulates, but also includes K01 strain (an isolated case observed in South Korea, see isolated cases)
Babesia parasites reproduce in red blood cells, where they can be seen as cross-shaped inclusions (four merozoites asexually budding, but attached forming a structure looking like a "Maltese cross")[11] and cause hemolytic anemia, quite similar to malaria.
------------
Only specialized laboratories can adequately diagnose Babesia infection in humans, so Babesia infections are considered highly under-reported. [...] It develops in patients who live in or travel to an endemic area or receive a contaminated blood transfusion within the preceding 9 weeks, so this aspect of the medical history is vital.[13] Babesiosis may be suspected when a person with such an exposure history develops persistent fevers and hemolytic anemia. The definitive diagnostic test is the identification of parasites on a Giemsa-stained thin-film blood smear.[13]
------------
"""
¶TICKS— Tick-borne Relapsing Fever (TBRF)
https://doh.wa.gov/you-and-your-family/illness-and-disease-z/tick-borne-relapsing-fever
"""
Soft tick relapsing fever is caused by Borrelia hermsii, Borrelia turicatae, and some other Borrelia species and transmitted by the bite of infected soft ticks of the genus Ornithodoros.
[...]
The ticks that can transmit STRF are called "soft ticks" and are different from "hard ticks" that transmit other diseases such as Lyme disease, Rocky Mountain spotted fever, and HTRF. Soft ticks bite and feed for much shorter periods of time, typically less than 30 minutes, and usually at night. They live within rodent nests and burrows, rather than grassy or bushy areas. Soft ticks prefer to feed on rodents but may seek out humans if rodents are scarce. Their bites are painless and most people don't realize that they have been bitten.
"""
https://en.wikipedia.org/wiki/Relapsing_fever
"""
Most infected people develop sickness between 5 and 15 days after they are bitten. The symptoms may include a sudden fever, chills, headaches, muscle or joint aches, and nausea. A rash may also occur. These symptoms usually continue for 2 to 9 days, then disappear. This cycle may continue for several weeks if the person is not treated.[4]
"""
https://doh.wa.gov/you-and-your-family/illness-and-disease-z/tick-borne-relapsing-fever
"""
Soft tick relapsing fever is caused by Borrelia hermsii, Borrelia turicatae, and some other Borrelia species and transmitted by the bite of infected soft ticks of the genus Ornithodoros.
[...]
The ticks that can transmit STRF are called "soft ticks" and are different from "hard ticks" that transmit other diseases such as Lyme disease, Rocky Mountain spotted fever, and HTRF. Soft ticks bite and feed for much shorter periods of time, typically less than 30 minutes, and usually at night. They live within rodent nests and burrows, rather than grassy or bushy areas. Soft ticks prefer to feed on rodents but may seek out humans if rodents are scarce. Their bites are painless and most people don't realize that they have been bitten.
"""
https://en.wikipedia.org/wiki/Relapsing_fever
"""
Most infected people develop sickness between 5 and 15 days after they are bitten. The symptoms may include a sudden fever, chills, headaches, muscle or joint aches, and nausea. A rash may also occur. These symptoms usually continue for 2 to 9 days, then disappear. This cycle may continue for several weeks if the person is not treated.[4]
"""
¶TICKS— B. miyamotoi → Borrelia miyamotoi disease (BMD)
hard ticks!
"""
Unlike B. burgdoferi, B. miyamotoi exhibits transovarial transmission, whereby the bacterium is passed from an adult tick directly into the eggs of new larvae within the ovaries. This mode of transmission has implications for diagnosis of disease because a very small larva can attach to a human host and go undetected.[1]
[...]
Treatment currently follows that of Lyme disease
[...]
BMD presents approximately two weeks after infection with non-specific flu-like symptoms including a relapsing-remitting fever in excess of 40C (104F), malaise, myalgias (muscle pain), arthralgias (joint pain), nausea, vomiting, and headache. Some patients may have elevated liver transaminases, thrombocytopenia, and leukopenia.[1][2][5][6] Cases involving an erythema migrans rash, which is a classic feature of Lyme disease, have been reported, but are believed to likely be the result of co-infection with B. burgdorferi and the development of co-morbid Lyme disease.[2] B. miyamotoi has also demonstrated a slower onset neurological syndrome including meningitis in some immunocompromised patients.[2][5]
[...]
Since ticks in all phases of their life cycle, including very small larvae, can transmit the disease to humans, the bite and tick can easily go undetected.[1] B. miyamotoi also transmits faster than B. burgdorfi, often within 24 hours of tick attachment.[1][2]
"""
https://en.wikipedia.org/wiki/Borrelia_miyamotoi
hard ticks!
"""
Unlike B. burgdoferi, B. miyamotoi exhibits transovarial transmission, whereby the bacterium is passed from an adult tick directly into the eggs of new larvae within the ovaries. This mode of transmission has implications for diagnosis of disease because a very small larva can attach to a human host and go undetected.[1]
[...]
Treatment currently follows that of Lyme disease
[...]
BMD presents approximately two weeks after infection with non-specific flu-like symptoms including a relapsing-remitting fever in excess of 40C (104F), malaise, myalgias (muscle pain), arthralgias (joint pain), nausea, vomiting, and headache. Some patients may have elevated liver transaminases, thrombocytopenia, and leukopenia.[1][2][5][6] Cases involving an erythema migrans rash, which is a classic feature of Lyme disease, have been reported, but are believed to likely be the result of co-infection with B. burgdorferi and the development of co-morbid Lyme disease.[2] B. miyamotoi has also demonstrated a slower onset neurological syndrome including meningitis in some immunocompromised patients.[2][5]
[...]
Since ticks in all phases of their life cycle, including very small larvae, can transmit the disease to humans, the bite and tick can easily go undetected.[1] B. miyamotoi also transmits faster than B. burgdorfi, often within 24 hours of tick attachment.[1][2]
"""
https://en.wikipedia.org/wiki/Borrelia_miyamotoi
¶[r!!**] PROTOCOL— Check for ticks!
"""
* Use an insect repellent containing DEET or picaridin and
* examine your skin for possible bites (especially behind the ears, on the back of the head, in the groin, armpits and behind the knees) following these activities.
"""
"""
* Use an insect repellent containing DEET or picaridin and
* examine your skin for possible bites (especially behind the ears, on the back of the head, in the groin, armpits and behind the knees) following these activities.
"""
¶VAX— Anti-tick vaccines, developed by Cuba ... "Gavac" (for animals)
documented here (great study on ticks in Cuba!):
https://www.mdpi.com/2076-0817/9/8/616
documented here (great study on ticks in Cuba!):
https://www.mdpi.com/2076-0817/9/8/616
¶Ticks @ Cuba
https://pmc.ncbi.nlm.nih.gov/articles/PMC7459505/
"""
Ticks and the vast array of pathogens they transmit, including bacteria, viruses, protozoa, and helminths, constitute a growing burden for human and animal health worldwide. In Cuba, the major tropical island in the Caribbean, ticks are an important cause of vector-borne diseases affecting livestock production, pet animal health and, to a lesser extent, human health. The higher number of tick species in the country belong to the Argasidae family and, probably less known, is the presence of an autochthonous tick species in the island, Ixodes capromydis. Herein, we provide a comprehensive review of the ticks and tick-borne pathogens (TBPs) affecting animal and human health in Cuba. The review covers research results including ecophysiology of ticks, the epidemiology of TBPs, and the diagnostic tools used currently in the country for the surveillance of TBPs. We also introduce the programs implemented in the country for tick control and the biotechnology research applied to the development of anti-tick vaccines.
"""
http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2304-01062021000200020
"""
Hard ticks are hematophagous ectoparasites, vectors of emerging zoonotic pathogens. Until 2011, there was evidence of infection/exposure to Borrelia burgdorferi in humans in Cuba, but the circulation of other agents is unknown. Aim: implement new diagnostic tools, explore infection/exposure of humans to tick-borne pathogens, their presence in vectors and level of knowledge in medical personnel.
"""
###
https://revistaccuba.sld.cu/index.php/revacc/article/view/860
"""
Introducción: Las garrapatas duras son ectoparásitos hematófagos, vectores de patógenos zoonóticos emergentes. Hasta 2011 en Cuba existían evidencias de infección/exposición a Borrelia burgdorferi en seres humanos, pero se desconoce sobre la circulación de otros agentes. Objetivo: implementar nuevas herramientas diagnósticas, explorar infección/exposición de seres humanos a patógenos transmitidos por garrapatas, presencia de estos en vectores y nivel de conocimientos en personal médico.
Métodos: se implementó PCR múltiple para detección de B. burgdorferi sl-Anaplasma spp. -Babesia spp., PCR para Borrelia spp., e infección artificial de garrapatas. Se describió la positividad a infección por B. burgdorferi (2011-2018), se exploró la presencia de anticuerpos contra borrelias en donantes de sangre de una región de baja exposición, anticuerpos contra otros agentes zoonóticos en población de riesgo, presencia de estos agentes en garrapatas, así como el nivel de conocimientos sobre enfermedad de Lyme en médicos.
Resultados: Se fortalecieron capacidades del IPK para detección molecular de patógenos transmitidos por garrapatas. Se encontraron nuevas evidencias serológicas de infección por B. burgdorferi en pacientes con sospechas de enfermedad de Lyme. Se demostró ausencia de anticuerpos específicos contra B. burgdorferi en donantes de sangre. Se encontraron evidencias de anticuerpos contraAnaplasma phagocytophilum, Ehrlichia chaffeensis y Babesia microti. Se demostró presencia de Anaplasma spp., Babesia spp., Rickettsia amblyommii y Coxiella burnetii en garrapatas. Se constataron conocimientos insuficientes sobre enfermedad de Lyme en personal médico. Conclusiones: estos resultados alertan a las autoridades nacionales de salud pública y personal médico sobre el riesgo de infección en individuos expuestos a picaduras de garrapatas.
"""
###
https://pmc.ncbi.nlm.nih.gov/articles/PMC7459505/
"""
Ticks and the vast array of pathogens they transmit, including bacteria, viruses, protozoa, and helminths, constitute a growing burden for human and animal health worldwide. In Cuba, the major tropical island in the Caribbean, ticks are an important cause of vector-borne diseases affecting livestock production, pet animal health and, to a lesser extent, human health. The higher number of tick species in the country belong to the Argasidae family and, probably less known, is the presence of an autochthonous tick species in the island, Ixodes capromydis. Herein, we provide a comprehensive review of the ticks and tick-borne pathogens (TBPs) affecting animal and human health in Cuba. The review covers research results including ecophysiology of ticks, the epidemiology of TBPs, and the diagnostic tools used currently in the country for the surveillance of TBPs. We also introduce the programs implemented in the country for tick control and the biotechnology research applied to the development of anti-tick vaccines.
"""
http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2304-01062021000200020
"""
Hard ticks are hematophagous ectoparasites, vectors of emerging zoonotic pathogens. Until 2011, there was evidence of infection/exposure to Borrelia burgdorferi in humans in Cuba, but the circulation of other agents is unknown. Aim: implement new diagnostic tools, explore infection/exposure of humans to tick-borne pathogens, their presence in vectors and level of knowledge in medical personnel.
"""
###
https://revistaccuba.sld.cu/index.php/revacc/article/view/860
"""
Introducción: Las garrapatas duras son ectoparásitos hematófagos, vectores de patógenos zoonóticos emergentes. Hasta 2011 en Cuba existían evidencias de infección/exposición a Borrelia burgdorferi en seres humanos, pero se desconoce sobre la circulación de otros agentes. Objetivo: implementar nuevas herramientas diagnósticas, explorar infección/exposición de seres humanos a patógenos transmitidos por garrapatas, presencia de estos en vectores y nivel de conocimientos en personal médico.
Métodos: se implementó PCR múltiple para detección de B. burgdorferi sl-Anaplasma spp. -Babesia spp., PCR para Borrelia spp., e infección artificial de garrapatas. Se describió la positividad a infección por B. burgdorferi (2011-2018), se exploró la presencia de anticuerpos contra borrelias en donantes de sangre de una región de baja exposición, anticuerpos contra otros agentes zoonóticos en población de riesgo, presencia de estos agentes en garrapatas, así como el nivel de conocimientos sobre enfermedad de Lyme en médicos.
Resultados: Se fortalecieron capacidades del IPK para detección molecular de patógenos transmitidos por garrapatas. Se encontraron nuevas evidencias serológicas de infección por B. burgdorferi en pacientes con sospechas de enfermedad de Lyme. Se demostró ausencia de anticuerpos específicos contra B. burgdorferi en donantes de sangre. Se encontraron evidencias de anticuerpos contraAnaplasma phagocytophilum, Ehrlichia chaffeensis y Babesia microti. Se demostró presencia de Anaplasma spp., Babesia spp., Rickettsia amblyommii y Coxiella burnetii en garrapatas. Se constataron conocimientos insuficientes sobre enfermedad de Lyme en personal médico. Conclusiones: estos resultados alertan a las autoridades nacionales de salud pública y personal médico sobre el riesgo de infección en individuos expuestos a picaduras de garrapatas.
"""
###
¶RESEARCH— Neglected Tropical Diseases
https://en.wikipedia.org/wiki/London_Declaration_on_Neglected_Tropical_Diseases
"""
The rather commitments include:
###
https://en.wikipedia.org/wiki/London_Declaration_on_Neglected_Tropical_Diseases
"""
The rather commitments include:
- eradicating or controlling transmission of Guinea worm disease
- eliminating lymphatic filariasis, leprosy, African sleeping sickness and blinding trachoma
- control of schistosomiasis, soil-transmitted helminthiasis, Chagas disease, visceral leishmaniasis, and river blindness by 2020.[5]
###
¶[!!*] Vibrio vulnificus (shellfish-bourne flash-eating bacteria)
"""i heard about a flash eating bacteria you get from handling crab or shellfish, and our body doesn't fight it well"""
Incidence: ###
↓
↓ deepseek
↓
"""
You're likely referring to Vibrio vulnificus, a dangerous bacterium that can cause severe infections, especially in people with compromised immune systems. Here's what you should know:
Key Facts About Vibrio vulnificus:
✔ Avoid raw/undercooked shellfish (especially if immunocompromised).
✔ Wear protective gloves when handling crabs/shellfish if you have cuts.
✔ Rinse wounds immediately after contact with seawater or seafood.
✔ Seek emergency care fast if you develop sudden redness, swelling, or fever after exposure.
"""
"""i heard about a flash eating bacteria you get from handling crab or shellfish, and our body doesn't fight it well"""
Incidence: ###
↓
↓ deepseek
↓
"""
You're likely referring to Vibrio vulnificus, a dangerous bacterium that can cause severe infections, especially in people with compromised immune systems. Here's what you should know:
Key Facts About Vibrio vulnificus:
- Source:
- Found in warm coastal waters, especially in shellfish (oysters, crabs, clams) and seawater.
- Enters the body through:
- Eating raw/undercooked shellfish.
- Open wounds exposed to seawater or handling shellfish.
- Why the Body Struggles to Fight It:
- It multiplies rapidly and produces toxins that damage tissue.
- People with liver disease, diabetes, or weakened immune systems are at much higher risk.
- Symptoms & Danger:
- Wound Infection: Painful, red, swollen skin that can quickly turn into necrotizing fasciitis ("flesh-eating" infection).
- Septicemia (Blood Infection): Fever, chills, low blood pressure, blistering skin lesions (often fatal if untreated).
- Gastrointestinal Illness: Vomiting, diarrhea, abdominal pain (from eating contaminated seafood).
- Urgency of Treatment:
- Requires immediate antibiotics (e.g., doxycycline + ceftazidime) and sometimes surgical debridement to remove dead tissue.
- 50% mortality rate if bloodstream infection occurs.
✔ Avoid raw/undercooked shellfish (especially if immunocompromised).
✔ Wear protective gloves when handling crabs/shellfish if you have cuts.
✔ Rinse wounds immediately after contact with seawater or seafood.
✔ Seek emergency care fast if you develop sudden redness, swelling, or fever after exposure.
"""
¶(identifying biting flies / black flies under microscope)
(closing)
https://scontent.flju1-1.fna.fbcdn.net/v/t1.6435-9/131639539_1790531564456831_3148256982675599548_n.jpg?_nc_cat=107&ccb=1-7&_nc_sid=f727a1&_nc_ohc=zUGdI8AA2QwQ7kNvwHDlUaB&_nc_oc=AdkTJAFJXIETrWZOKNiCQus1KCmUhNMLBvgnscwrLd1UdI-_cytdB0tNH6tpZjAZrGE&_nc_zt=23&_nc_ht=scontent.flju1-1.fna&_nc_gid=Ybr2B28QwpjepWlh3WchRA&oh=00_AfPvASNTNePRvxr5UHGJ17W5niggYWF2fUXlhGmESYeY0g&oe=687CCAC3
https://www.researchgate.net/figure/Morphological-features-of-black-fly-adults-A-female-head-front-view-B-thorax-and_fig1_233727136
https://extension.entm.purdue.edu/publichealth/insects/blackfly.html
<----------------------------------- ((new))
http://www.cubadebate.cu/especiales/2025/04/06/enfermedades-zoonoticas-algo-sobre-lo-que-usted-debe-conocer/
"75% diseases comes via (zoonotic transmission from) animals"
###
(closing)
https://scontent.flju1-1.fna.fbcdn.net/v/t1.6435-9/131639539_1790531564456831_3148256982675599548_n.jpg?_nc_cat=107&ccb=1-7&_nc_sid=f727a1&_nc_ohc=zUGdI8AA2QwQ7kNvwHDlUaB&_nc_oc=AdkTJAFJXIETrWZOKNiCQus1KCmUhNMLBvgnscwrLd1UdI-_cytdB0tNH6tpZjAZrGE&_nc_zt=23&_nc_ht=scontent.flju1-1.fna&_nc_gid=Ybr2B28QwpjepWlh3WchRA&oh=00_AfPvASNTNePRvxr5UHGJ17W5niggYWF2fUXlhGmESYeY0g&oe=687CCAC3
https://www.researchgate.net/figure/Morphological-features-of-black-fly-adults-A-female-head-front-view-B-thorax-and_fig1_233727136
https://extension.entm.purdue.edu/publichealth/insects/blackfly.html
<----------------------------------- ((new))
http://www.cubadebate.cu/especiales/2025/04/06/enfermedades-zoonoticas-algo-sobre-lo-que-usted-debe-conocer/
"75% diseases comes via (zoonotic transmission from) animals"
###